Osteoarthritis Risk Estimator
How likely is osteoarthritis?
Answer these questions to estimate your risk level and see early intervention benefits
Your Risk Assessment
Early Intervention Benefits
When you hear the term Osteoarthritis is a degenerative joint disease that slowly wears down the cartilage cushioning the ends of bones, you might think it’s something that only shows up when you’re already in pain. The truth is, catching it early can change the whole trajectory of the condition. In this guide we’ll walk through the warning signs, how doctors confirm the diagnosis, and why acting fast makes a big difference for your joints and daily life.
Key Takeaways
- Early signs include stiffness after inactivity, joint swelling and subtle aching that worsens with use.
- Professional diagnosis relies on a mix of physical exam, imaging (X‑ray, MRI) and, increasingly, biomarkers.
- Interventions such as weight management, targeted physiotherapy and selective NSAIDs can halt or slow damage when started early.
- Delaying treatment often leads to higher pain scores, reduced mobility, and a greater chance of needing joint replacement.
- Regular monitoring and lifestyle tweaks keep the disease in check and preserve quality of life.
Spotting Osteoarthritis Early
Most people associate osteoarthritis with creaky knees after decades of use, but the condition often begins subtly. Look out for these cues:
- Morning stiffness lasting less than 30 minutes. A brief achy feeling that eases after moving is classic.
- Joint swelling that appears after activity or at the end of the day.
- Occasional grinding or clicking sensations.
- Loss of flexibility in the affected joint, especially after sitting for long periods.
If any of these symptoms persist for more than a few weeks, it’s worth scheduling a check‑up. Early detection is especially crucial for people with known risk factors such as obesity, previous joint injury, or a family history of osteoarthritis.

How Doctors Diagnose Osteoarthritis
The diagnostic pathway blends patient history, a physical exam, and imaging. Here’s what typically happens:
- Clinical evaluation: The clinician assesses range of motion, checks for tenderness, and notes any swelling.
- Plain radiography (X‑ray): An X‑ray reveals the classic signs-joint space narrowing, osteophyte (bone spur) formation, and subchondral sclerosis. Radiologists often grade severity using the Kellgren-Lawrence grading system (0‑4).
- Advanced imaging: When X‑rays are inconclusive, a MRI can visualize cartilage loss, meniscal tears, and inflammation of the synovial fluid layer.
- Laboratory tests: Blood work rules out inflammatory arthritis (like rheumatoid arthritis). Emerging research also tracks biomarkers such as CTX‑II to flag early cartilage breakdown.
Because plain X‑rays may miss early cartilage thinning, doctors increasingly rely on MRI and biomarker panels for a more proactive approach.
Why Early Intervention Works
Once the disease is caught before major cartilage loss, several therapeutic avenues are far more effective. Think of the joint as a car engine: fixing a minor oil leak early prevents catastrophic damage.
| Outcome | Early Intervention (within 6 months of symptoms) | Late Intervention (after 2+ years of symptoms) |
|---|---|---|
| Pain level (0‑10 scale) | 2‑4 | 6‑9 |
| Joint‑space loss progression (per year) | 0.2mm | 0.8mm |
| Need for total joint replacement (5‑year risk) | 12% | 38% |
| Quality‑of‑life score (SF‑36) | 78 | 55 |
The numbers above come from longitudinal studies conducted in the UK and North America, showing that patients who adopt lifestyle changes and targeted therapy early experience slower structural damage and stay active longer.
Core Interventions You Can Start Right Away
Early treatment isn’t about one magic pill; it’s a toolbox. Here are the pillars most clinicians recommend:
- Weight management: Reducing body weight by just 5% can lower knee‑joint load by 10‑15%, easing pain and slowing cartilage wear.
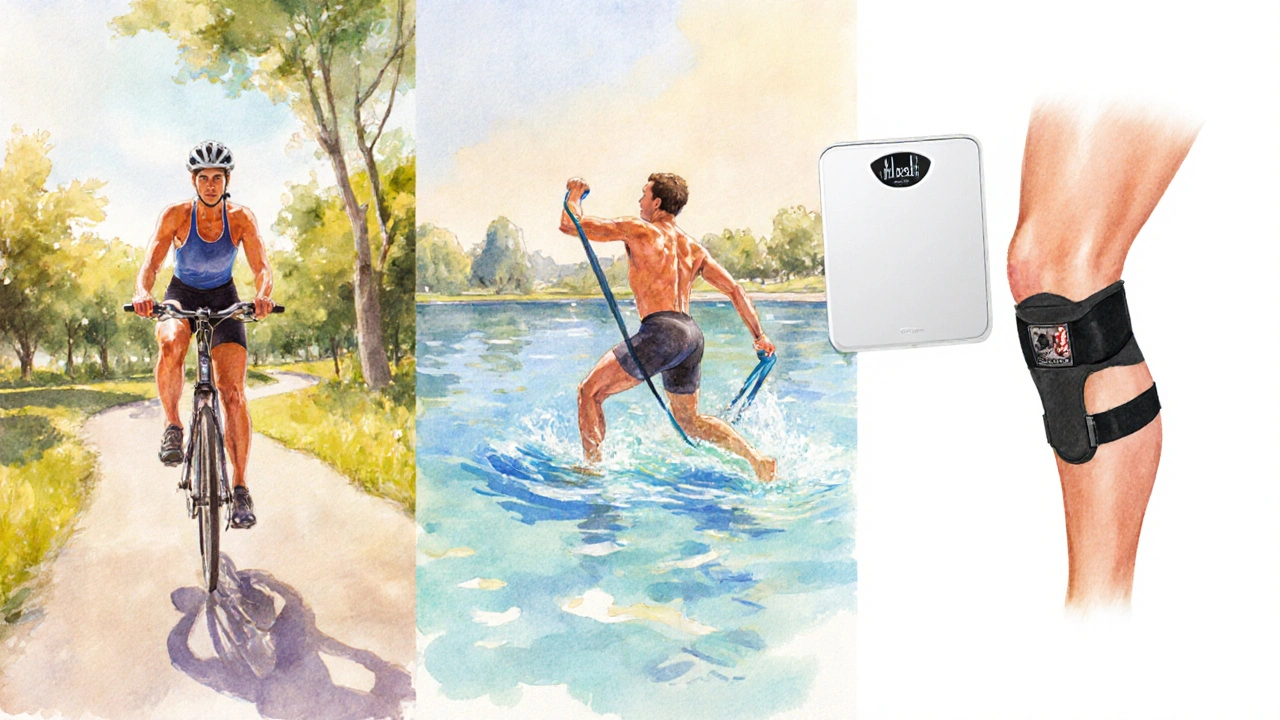
- Exercise and physiotherapy: A tailored program focusing on low‑impact aerobic activity (e.g., swimming, cycling) plus muscle‑strengthening for the quadriceps and hip abductors improves joint stability. Physiotherapy sessions also teach pain‑free movement patterns.
- Medication: Short courses of NSAIDs (ibuprofen, naproxen) relieve inflammation. For those who can’t tolerate NSAIDs, topical capsaicin or acetaminophen are viable alternatives.
- Supplements: Glucosamine and chondroitin have mixed evidence, but some patients report modest symptom relief when taken early.
- Joint protection aids: Braces or orthotics redistribute load during activities, especially for the knee and hip.
When these measures start soon after symptoms appear, they often keep pain at a manageable level for years without needing invasive procedures.
When More Advanced Therapies Become Necessary
If early steps don’t curb progression, doctors may discuss options like intra‑articular steroid injections, hyaluronic acid viscosupplementation, or emerging disease‑modifying osteoarthritis drugs (DMOADs). These treatments aim to protect cartilage and reduce inflammation, but they’re most successful when combined with the lifestyle foundations mentioned above.
In severe cases where joint damage is extensive, total joint replacement remains the gold‑standard solution. However, even then, patients who engaged in early intervention tend to recover faster and have better post‑surgical outcomes.
Practical Steps to Take Today
- Schedule a primary‑care visit if you notice persistent joint stiffness or swelling.
- Ask for a thorough physical exam and discuss getting an early X‑ray or MRI if symptoms are new.
- Start a low‑impact activity routine - aim for 150minutes a week of swimming, brisk walking, or cycling.
- Track your weight and consider a nutrition plan that emphasizes anti‑inflammatory foods (omega‑3 rich fish, leafy greens, nuts).
- Consult a physiotherapist for a personalized strengthening program.
- Keep a symptom diary to share with your doctor; it helps gauge treatment response.
Taking these actions now puts you in the driver’s seat of your joint health.
Frequently Asked Questions
What is the earliest sign of osteoarthritis?
The first clue is usually mild joint stiffness that eases after a few minutes of movement, often accompanied by a low‑grade ache after activity.
Can an X‑ray detect osteoarthritis in its early stages?
Plain X‑rays are great for spotting bone spurs and joint‑space narrowing, but they may miss early cartilage loss. MRI is more sensitive for detecting subtle changes before the X‑ray becomes abnormal.
Is weight loss really effective for knee osteoarthritis?
Yes. Studies show a 5% reduction in body weight can lower knee‑joint load by up to 15%, translating into less pain and slower disease progression.
Do supplements like glucosamine help if you start them early?
The evidence is mixed, but some early‑stage patients report modest symptom relief. It’s safest to discuss any supplement regimen with your clinician.
When is joint replacement considered?
Joint replacement is typically reserved for severe pain and functional loss that persist despite conservative measures, and when imaging shows extensive joint‑space collapse.
Remember, catching osteoarthritis early opens the door to a range of treatments that keep you moving, reduce pain, and delay the need for surgery. By staying vigilant about symptoms and acting quickly, you give your joints the best chance to stay healthy for years to come.


15 Responses
Early detection can change the game for osteoarthritis.
From a prognostic epistemology standpoint, the temporal latency of osteoarthritic manifestation demands a preemptive diagnostic schema. The integration of biomechanical biomarkers with patient-reported outcome measures constitutes a multimodal risk stratification paradigm. By calibrating the stochastic variance in joint loading patterns, clinicians can infer the probabilistic onset of cartilage degeneration. Moreover, the deployment of algorithmic risk estimators leverages Bayesian inference to refine predictive fidelity. Early intervention, therefore, operates as a modifiable variable within the causal network of disease progression. Synovial inflammation, when attenuated through physiotherapeutic regimens, alters the trajectory of extracellular matrix catabolism. Nutritional modulation of systemic adipokine profiles further mediates joint homeostasis. Empirical evidence underscores that weight reduction yields a quantifiable decrement in joint compressive forces, thereby decelerating erosive processes. The psychosocial dimension of patient empowerment engenders adherence to therapeutic protocols, enhancing longitudinal outcomes. In addition, the early adoption of lubricating intra-articular injections can restore viscoelastic properties of the synovial fluid milieu. The confluence of genetic predisposition and epigenetic expression patterns can be interrogated via genome-wide association studies to personalize preventive strategies. Patient stratification based on familial incidence augments the sensitivity of screening initiatives. The cost-effectiveness analyses reveal that early therapeutic engagement reduces cumulative healthcare expenditures. Consequently, a paradigm shift toward anticipatory care aligns with the broader objectives of value-based medicine. Ultimately, the synthesis of these multidisciplinary insights affirms the imperative of early diagnosis and intervention in osteoarthritis management.
While your exposition is impressively verbose, it obscures the practical reality that many patients lack access to such sophisticated screening tools. The moral imperative is to democratize early detection, not to entangle it in academic jargon.
It is alarming how pharmaceutical conglomerates may profit from delayed diagnoses, subtly engineering public complacency. The veil of clinical neutrality often shields agendas that prioritize market expansion over patient wellbeing.
Obviously the claim lacks substantiation and reeks of paranoia – no evidnce shows a coordinated effort to delay osteoarthritis care. It's simply the standard medical process, nothing conspiratorial.
Let's focus on actionable steps: encourage regular movement, maintain a healthy weight, and consult a physiotherapist early. These evidence‑based measures can markedly improve joint health.
Correction: the phrase should be “maintain a healthy weight,” not “maintain a healthy weight.” Additionally, “physiotherapist” is singular; “a physiotherapist” is appropriate.
Great points! Remember, each small healthy habit compounds over time, turning the odds in your favor.
Ah, yes, because obviously a handful of squats will magically reverse decades of joint wear – a truly cinematic solution.
You know, the discourse around osteoarthritis often suffers from a dearth of intellectual rigor; it’s high time we elevate the conversation beyond superficial advice.
Indeed, the commonplace recommendations lack the nuanced understanding that true experts possess, rendering them trivial at best.
This whole “early detection” hype is a profit‑driven gimmick; patients are fed nonsense while insurers reap the benefits.
I see your point, but could we also consider how early lifestyle changes might actually reduce long‑term costs for everyone?
The empirical data suggest that early intervention yields statistically significant improvements in functional outcomes 😊. Continued research is essential.
Absolutely! Leveraging predictive analytics and personalized rehab protocols can turbo‑charge recovery 🚀. Let’s keep pushing the envelope!