Blood Pressure Medication Adjustment Calculator
How This Works
Based on clinical data showing GLP-1 medications lower blood pressure by 4-6 mmHg systolic. This calculator estimates your potential blood pressure reduction and recommends safe dose adjustments based on your current medications and weight loss.
⚠️ Important Safety Note: This tool provides estimates only. Never adjust your medications without consulting your doctor. The FDA reports 27% more hypotension cases with GLP-1 drugs between 2021-2023.
Your Estimated Blood Pressure Changes
Estimated BP Reduction
Systolic: mmHg
Diastolic: mmHg
Total Potential Reduction
Systolic: mmHg
Diastolic: mmHg
Medication Adjustment Recommendations
Risk Assessment
Critical Warning: 22% of patients over 65 experience hypotension with GLP-1 drugs. Report dizziness, fainting, or extreme fatigue to your doctor immediately.
Based on data from clinical trials showing Wegovy lowers systolic BP by 6.2 mmHg and diastolic by 3.8 mmHg
When you start a weight loss medication like Wegovy or Saxenda, you’re not just trying to lose pounds-you’re changing how your whole body processes drugs, including the ones you take for high blood pressure or depression. It’s not a simple swap. These medications don’t just affect your appetite. They slow down your stomach, alter how your kidneys handle salt and water, and shift your blood pressure in ways that can be dangerous if you’re already on other meds. And if you’re taking antidepressants? That adds another layer most people don’t see coming.
How GLP-1 Medications Lower Blood Pressure (And Why That’s a Problem)
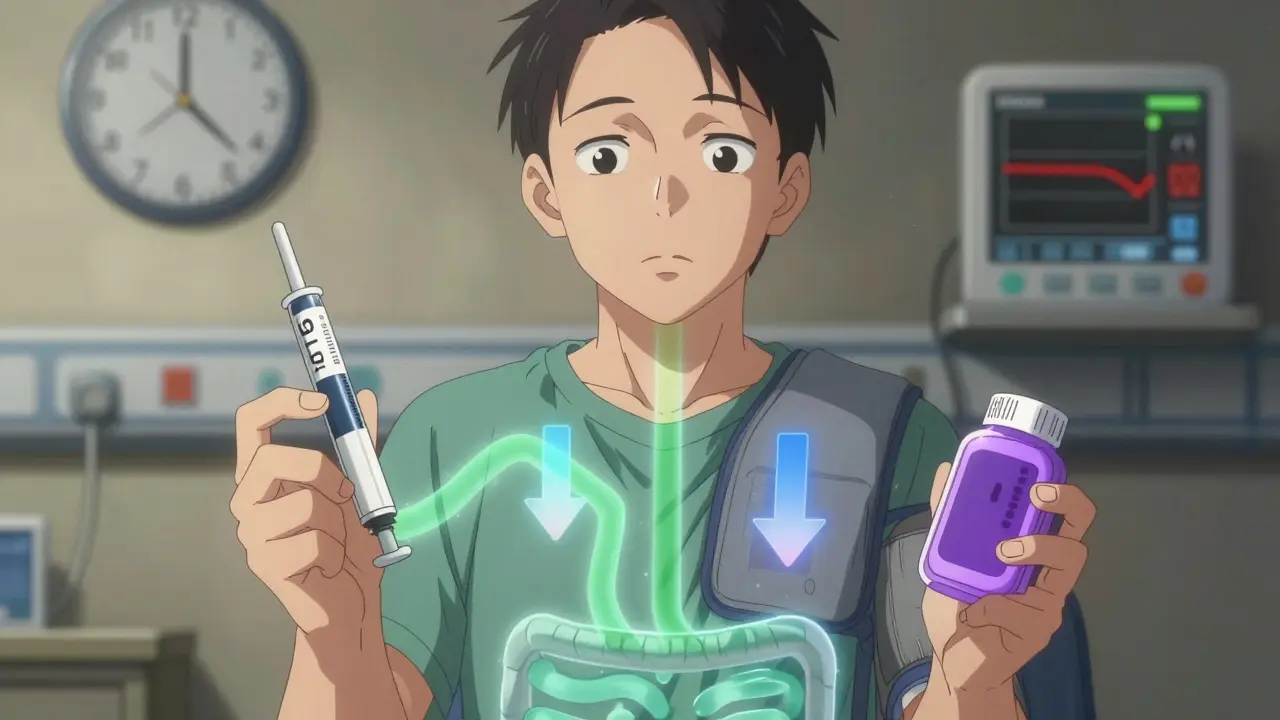
Wegovy (semaglutide) and Saxenda (liraglutide) are part of a class called GLP-1 receptor agonists. They work by mimicking a natural hormone that tells your brain you’re full. But they also slow down how fast food leaves your stomach-by 25% to 35%. That’s great for curbing cravings, but it’s a problem for medications you swallow. If your blood pressure pills are absorbed slower, they might not work right. Worse, these drugs cause real, measurable drops in blood pressure.
Clinical trials show Wegovy lowers systolic blood pressure by an average of 6.2 mmHg and diastolic by 3.8 mmHg. Saxenda’s effect is smaller but still significant: about 4.1 mmHg systolic drop. For someone with normal blood pressure, that’s fine. For someone on lisinopril, losartan, or a beta-blocker? It can push them into hypotension-blood pressure below 90/60 mmHg. That means dizziness, fainting, fatigue. In one study, 12% to 18% of patients on GLP-1 meds and blood pressure drugs experienced this. Among people over 65, the rate jumped to 22%.
And it’s not just the medication itself. Losing weight lowers blood pressure naturally. Lose 10% of your body weight? That alone can drop systolic pressure by 5-10 mmHg. Now add the drug’s effect on your stomach and kidneys, and you’ve got a double hit. Many patients end up needing their blood pressure meds cut in half-or even stopped-within three months of starting Wegovy or Saxenda.
Which Blood Pressure Drugs Are Most Affected?
Not all blood pressure medications react the same way. ACE inhibitors like enalapril and lisinopril, and ARBs like losartan, are the biggest concern. When combined with GLP-1 drugs, they increase the risk of low blood pressure and, oddly, high potassium levels (hyperkalemia). Why? Because weight loss improves kidney function, but GLP-1 meds can reduce blood flow to the kidneys just enough to mess with how they filter potassium. This combo raises hyperkalemia risk by 15-22%.
Diuretics like hydrochlorothiazide or furosemide make things worse. They already pull fluid out of your body. Add a GLP-1 drug that slows digestion and lowers blood pressure, and you’re more likely to get dehydrated, dizzy, or even pass out. One study found that combining diuretics with GLP-1 meds increased blood pressure-lowering effects by 25-40%.
On the flip side, beta-blockers and calcium channel blockers don’t interact as strongly. But that doesn’t mean they’re safe. If your blood pressure drops suddenly, any medication that slows your heart rate (like metoprolol) can make you feel worse. The key isn’t avoiding certain drugs-it’s adjusting doses as you lose weight.
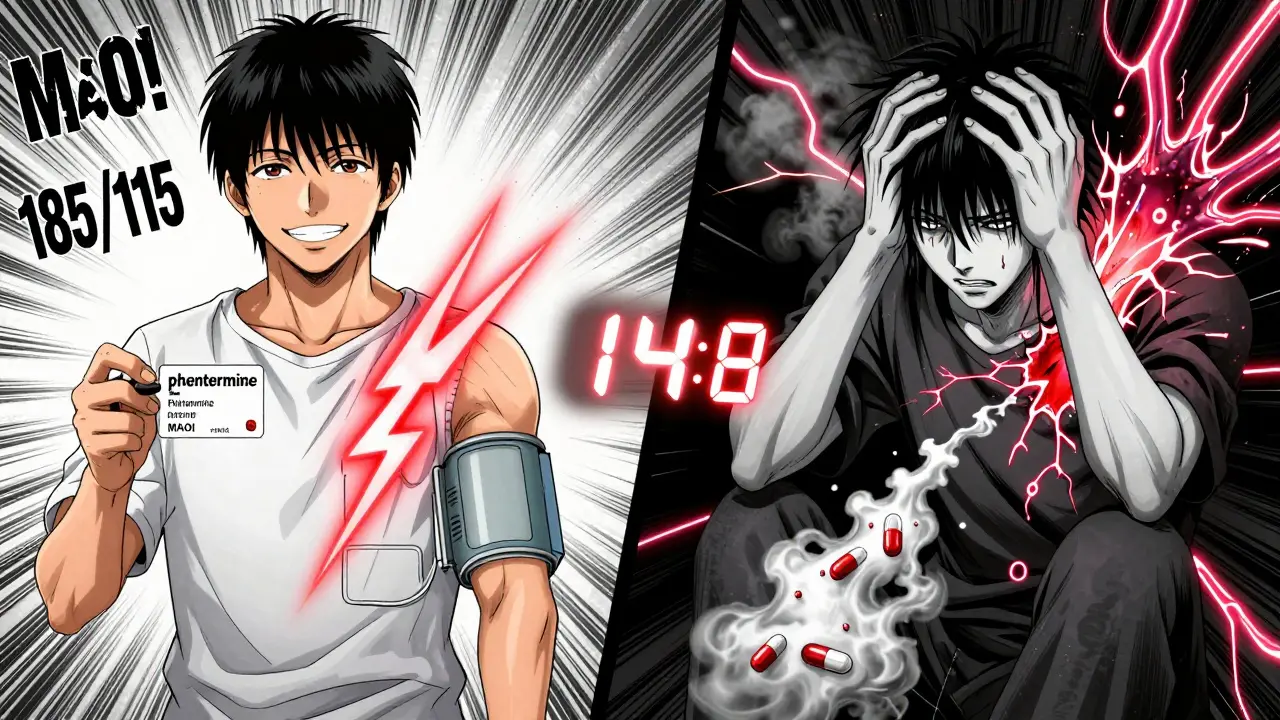
Phentermine: The Opposite Problem
If you’re on phentermine, the story flips. This older stimulant works like amphetamines-it increases norepinephrine, which tightens blood vessels and raises heart rate. It can push systolic blood pressure up by 5-15 mmHg and diastolic by 3-10 mmHg. That’s dangerous if you already have hypertension. The CDC says over 107 million U.S. adults have high blood pressure. For them, phentermine can turn a manageable condition into a crisis.
The worst-case scenario? Combining phentermine with MAOIs, a type of antidepressant. This combo can trigger a hypertensive crisis-blood pressure spiking over 180/120 mmHg. The FDA has documented emergency room visits from this interaction. In some cases, pressure hit 220/120. That’s a stroke or heart attack away. That’s why you must stop MAOIs at least 14 days before starting phentermine. No exceptions.
Qsymia (phentermine-topiramate) is a middle ground. Topiramate lowers blood pressure, so it balances phentermine’s rise. Still, 30% of users see a net increase in pressure. It’s not risk-free.

Antidepressants and Delayed Absorption
Here’s the part most doctors don’t warn you about: GLP-1 meds can make your antidepressants stop working. Not because they cancel each other out-but because your stomach moves slower. SSRIs like sertraline, fluoxetine, and escitalopram are absorbed in the upper intestine. If food and pills sit in your stomach longer, less of the drug reaches your bloodstream.
One study found sertraline absorption dropped by 18-25% when taken with liraglutide. Patients reported their anxiety or depression creeping back. On Reddit, users described feeling like their meds “stopped working” after starting Wegovy. One woman had to increase her sertraline dose by 50% just to feel stable again.
It’s not just SSRIs. SNRIs like venlafaxine and tricyclics like amitriptyline can be affected too. The fix? Space out your doses. Take your antidepressant at least two hours before or after your GLP-1 shot. That gives your stomach time to empty before the next dose slows things down again. Psychiatrists who track this now routinely ask patients if they’re on weight loss meds when depression symptoms return.
What You Should Do
If you’re on blood pressure or antidepressant meds and considering a weight loss drug, don’t guess. Here’s what actually works:
- Get your blood pressure checked before starting any weight loss medication. Write it down.
- Check your current meds with your doctor. Don’t assume your pharmacist caught it.
- Expect to adjust your blood pressure meds within the first 6-8 weeks. Many need a 25-50% reduction.
- Monitor for dizziness, fainting, or extreme fatigue-especially when standing up.
- If you’re on an SSRI and feel worse after starting Wegovy or Saxenda, talk to your psychiatrist. It might be absorption, not relapse.
- Avoid phentermine if you have uncontrolled hypertension or are on MAOIs. Period.
Weight loss is a goal. But if you lose 20 pounds and end up in the ER from low blood pressure or a panic attack because your antidepressant isn’t working, you didn’t win. You just traded one problem for another.
The Bigger Picture
The GLP-1 weight loss market hit $18.7 billion in 2023. Prescriptions for Wegovy jumped 320% in a year. That’s good news for people struggling with obesity. But it’s also a warning sign. More people are taking these drugs than ever-and more are having dangerous interactions. The FDA received 27% more reports of hypotension from these meds between 2021 and 2023.
Doctors are catching on. 41% of cardiologists now consult obesity specialists before prescribing both types of meds. That’s up from 19% in 2020. By 2025, most electronic health records will flag risky combos automatically. But until then, you have to be your own advocate.
Don’t wait for your doctor to ask. Bring up your meds. Say: “I’m starting Wegovy. What should I do about my lisinopril and sertraline?” If they shrug, find someone who knows the science. This isn’t just about weight. It’s about keeping your heart, brain, and body safe while you change.
Can I take Wegovy with my blood pressure pills?
Yes, but your dose may need to be lowered. Wegovy lowers blood pressure, and combining it with ACE inhibitors, ARBs, or diuretics can cause dangerous drops. Most patients need a 25-50% reduction in their blood pressure meds within the first 3 months. Always check your pressure weekly for the first month and report dizziness or fainting to your doctor.
Will Saxenda make my antidepressants stop working?
It can. Saxenda slows stomach emptying, which reduces how much of your antidepressant (like sertraline or fluoxetine) gets into your bloodstream. Some people notice their anxiety or depression returning. The fix: take your antidepressant at least 2 hours before your Saxenda injection. If symptoms persist, your psychiatrist may need to adjust your dose.
Is phentermine safe if I have high blood pressure?
No-not if your blood pressure isn’t well controlled. Phentermine raises blood pressure by stimulating your nervous system. It can push systolic pressure up by 15 mmHg or more. If you’re on blood pressure meds, it can interfere with their effect. And never take it with MAOIs-it can cause a life-threatening spike in blood pressure. Talk to your doctor about safer alternatives like GLP-1 medications.
How long should I wait after stopping an MAOI before starting phentermine?
You must wait at least 14 days. MAOIs stay in your system for up to two weeks. Starting phentermine too soon can cause a hypertensive crisis-blood pressure over 180/120 mmHg-with symptoms like severe headache, chest pain, or blurred vision. This is a medical emergency. Always follow your doctor’s exact timeline.
Do I need to stop my blood pressure meds if I start Wegovy?
Not necessarily, but most people need a dose reduction. Losing weight and the drug’s effect on your body often lower blood pressure more than expected. About 63% of endocrinologists reduce ACE inhibitor or ARB doses by 25-50% when starting GLP-1 therapy. Never stop or change your meds without medical supervision. Monitor your pressure daily and report symptoms like lightheadedness.
What’s Next
Research is moving fast. A major NIH trial called PRECISION-OBESITY is testing whether your genes can help predict how much your blood pressure will drop on GLP-1 meds. By 2025, AI tools in electronic health records will likely auto-flag dangerous combos before you even leave the clinic. But right now, the responsibility is on you. Keep a log: your weight, your blood pressure readings, your mood, your meds. Share it with your doctor. Don’t assume they know everything. You’re not just a patient-you’re the expert on your own body.

9 Responses
i started wegovy last month and my bp dropped so fast i nearly passed out getting out of the shower. my doctor had to cut my lisinopril in half. weirdly, i didn’t even realize how bad the dizziness was until it stopped. now i just feel normal. also, my sertraline felt like it stopped working for a bit-like my anxiety came back outta nowhere. turned out my stomach was just moving too slow. started taking it 2 hours before my shot and boom, back to baseline. don’t ignore this stuff.
they dont want you to know this but the pharmaceutical companies are pushing these drugs because they know people will need more meds to fix the side effects they create. glp-1s are just the beginning. soon youll need blood pressure meds antidepressants potassium pills diuretics and maybe even a pacemaker just to survive the weight loss journey. its a profit machine. the fda knows. your doctor knows. they just dont tell you. i read the clinical trial fine print. its not medicine its a trap. and now im paranoid every time i take a pill.
man i just started saxenda and my mom asked if i was okay because i kept sitting down suddenly. turns out my bp was 88 over 56. i thought i was just tired. now i check it every morning. also my antidepressant feels weaker so i take it before my injection now. no drama just real talk. if you’re on this stuff keep a log. your future self will thank you.
the fact that you need to time your antidepressant intake around a GLP-1 agonist’s gastric emptying kinetics suggests we’ve entered a new era of polypharmacy where pharmacokinetic optimization supersedes clinical intuition. most prescribers are still operating on 2010 guidelines. the data is clear: delayed absorption isn’t anecdotal-it’s a pharmacodynamic phenomenon with measurable AUC reductions. if your psychiatrist isn’t aware of this, you’re being undermanaged.
so you’re telling me the same people who told us fat people just needed to eat less and move more are now selling us drugs that mess with our brain chemistry and kidneys? classic. and now we’re supposed to be grateful? the whole system is rigged. you lose weight and suddenly your meds don’t work. you get dizzy. you feel like crap. but hey at least you’re thin right? the real crime is that they never told us this would happen before we signed up. this isn’t health care. this is exploitation dressed up as science.
you are not alone. i was scared too. but you took the first step. that’s brave. your body is changing. your mind is changing. and your meds might need adjusting. that doesn’t mean you failed. it means you’re learning. talk to your doctor. write things down. take care of yourself. you are doing better than you think. one day at a time. you’ve got this.
the pharmacokinetic interaction between GLP-1 RAs and renin-angiotensin-aldosterone system inhibitors is mediated by reduced glomerular filtration rate and altered sodium handling secondary to volume depletion. concomitant use with diuretics exacerbates this via additive hypotensive effects. serum potassium elevation occurs due to decreased aldosterone sensitivity in distal nephron segments. concurrent SSRI absorption is compromised due to delayed gastric emptying, reducing Cmax and delaying Tmax. clinical management requires titration of antihypertensives and temporal separation of oral psychotropics.
why are we even doing this? just eat less. move more. stop taking so many pills. why does everything have to be so complicated? now i gotta time my meds? check my bp every day? this is ridiculous. i just wanted to lose weight. not become a pharmacist.
okay, so let me get this straight: you’re telling me that if I’m on an SSRI and I start a GLP-1 agonist, my medication absorption is compromised not because of a drug-drug interaction at the receptor level, but because of a mechanical delay in gastric emptying-which then reduces the bioavailability of my antidepressant, leading to a functional deficiency in serotonergic neurotransmission, which then manifests as a return of depressive or anxious symptoms that are misattributed to relapse, when in fact it’s a pharmacokinetic issue that can be resolved simply by staggering the timing of administration by two hours? And yet, 41% of cardiologists are now consulting obesity specialists? That’s not progress-that’s a systemic failure of interdisciplinary communication that’s been allowed to fester for years because no one wanted to admit that weight loss drugs aren’t just ‘weight loss drugs’-they’re neurometabolic disruptors with downstream effects on every major organ system. And now we’re expected to self-manage all of this while the FDA receives 27% more hypotension reports? This isn’t innovation. This is a public health experiment with no informed consent.