Vitamin E Intake Calculator for Warfarin Users
How Much Vitamin E Are You Taking?
Many people unknowingly exceed the safe limit of 400 IU daily when taking warfarin. This calculator helps you track your intake from supplements and food sources.
Your Daily Vitamin E Intake
Take vitamin E every day to support your skin and immune system. Meanwhile, you’re on warfarin to prevent dangerous blood clots. Sounds harmless, right? Vitamin E and warfarin might seem like a simple combo - but in reality, this pairing can quietly raise your risk of serious bleeding, even when you feel fine.
Why This Interaction Isn’t Just a Theory
Warfarin works by blocking vitamin K, a nutrient your body needs to make clotting proteins. Vitamin E, on the other hand, doesn’t directly affect vitamin K. But here’s the catch: it interferes with platelets - the tiny blood cells that help clots form. When you mix high doses of vitamin E with warfarin, you’re hitting the clotting system from two sides. One drug slows clotting. The other makes platelets less sticky. Together, they can turn a small cut into a slow bleed - or worse, cause internal bleeding without warning.
It’s not just speculation. In 2013, researchers studied over 1,000 patients on warfarin for atrial fibrillation. They found that those with higher blood levels of vitamin E had significantly more bleeding events - including brain bleeds. The risk jumped when vitamin E levels hit 4.49 μmol/mmol cholesterol. At 5.56 μmol/mmol cholesterol, the chance of a major bleed nearly doubled. These patients weren’t taking crazy doses - some were on just 800 IU daily. That’s less than what’s in many over-the-counter bottles.
The 800 IU Myth: Why Some Studies Say It’s Safe
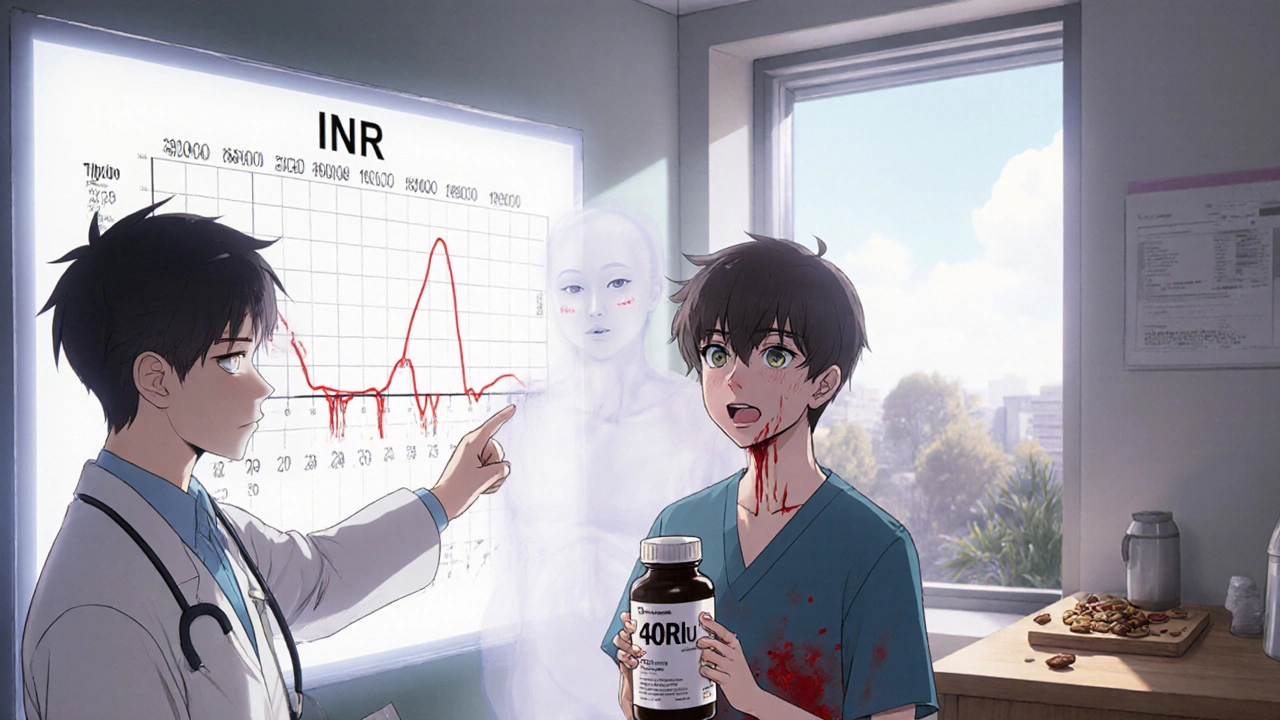
You might have heard that vitamin E is safe with warfarin. That’s based on a small 1996 study where 21 people took up to 800 IU of vitamin E daily for weeks. Their INR numbers didn’t change. No bleeding. Case closed, right?
Not so fast. That study was short. It looked at INR - a snapshot of clotting time - but didn’t track actual bleeding events. And it didn’t measure vitamin E levels in the blood. Later research showed that the danger doesn’t always show up in INR. Sometimes, it builds slowly. One case report described a patient who took 800 IU of vitamin E daily for four weeks. Everything looked normal. Then, out of nowhere, they started bleeding from the gums and nose. The vitamin E had quietly weakened their platelets. By the time INR rose, it was too late.
Even more troubling: a small unpublished study found that just 42 IU of vitamin E daily - less than a typical multivitamin - boosted anticoagulation in three volunteers. That suggests some people are far more sensitive than others. Genetics play a role. Variants in the CYP2C9 and VKORC1 genes affect how your body breaks down warfarin. If you have these variants, even low doses of vitamin E might push you into danger.
What Dose Is Dangerous?
There’s no universal safe dose - but there’s a clear red zone. Most guidelines agree: anything above 400 IU daily increases risk. The American College of Chest Physicians, the University of California San Diego Anticoagulation Service, and the American Heart Association all warn against doses higher than this. The European Society of Cardiology now recommends checking vitamin E levels in patients with unexplained bleeding.
But here’s the problem: supplement labels lie. A bottle labeled “400 IU” might contain 600 IU. There’s no strict FDA oversight for supplements. A 2022 NIH update said the evidence is mixed - but added, “caution is warranted, particularly at doses exceeding 400 IU daily.” That’s not a suggestion. It’s a warning.
Most people don’t realize how much vitamin E they’re getting. It’s in multivitamins, fish oil blends, and skin creams. One daily multivitamin can give you 134 IU. Add a separate vitamin E capsule (200 IU), and you’re already at 334 IU - close to the danger line. Throw in a handful of almonds (7 IU each) and sunflower seeds (10 IU per ounce), and you’re approaching 400 IU without even trying.
What Do Clinics Actually Do?
Real-world practice doesn’t match the old studies. A 2017 survey of 250 anticoagulation clinics found that 78% routinely warn patients about vitamin E. Sixty-three percent specifically say: “Don’t go over 400 IU.”
If you insist on taking it anyway, clinics don’t just shrug. They require action:
- Baseline INR before starting vitamin E
- Weekly INR checks for the first month
- Biweekly checks after that
- Immediate recheck if you bruise easily, nosebleeds, or have dark stools
That’s 3 to 5 extra clinic visits a year - just for one supplement. And it’s not just inconvenient. Missed tests mean missed warnings. One patient in a 2019 case study bled into his abdomen after skipping his INR check for two weeks. He’d been taking 600 IU of vitamin E daily. His doctor never asked about supplements.
What About Other Supplements?
You’re not alone in taking vitamin E. It’s the third most popular single-ingredient supplement in the U.S., after vitamin D and fish oil. But you’re not just dealing with vitamin E. Many people also take fish oil, garlic, ginger, ginkgo, or turmeric - all of which can thin the blood. Combine them with vitamin E, and the risk multiplies.
For example: fish oil has its own antiplatelet effect. Taking 1,000 mg of fish oil daily with 400 IU of vitamin E and warfarin? That’s a triple threat. The American Heart Association specifically warned in 2009 that high-dose vitamin E increases the risk of hemorrhagic stroke - especially in people on anticoagulants. That’s not a footnote. It’s a headline.

What Should You Do?
Here’s the bottom line:
- If you’re on warfarin, avoid vitamin E supplements over 400 IU daily - period.
- Check your multivitamin. If it contains vitamin E, note the dose. Add it to any other supplement you take.
- Don’t assume “natural” means safe. Supplements aren’t tested like drugs.
- Tell your doctor about every pill, powder, or drop you take - even if you think it’s harmless.
- Don’t stop warfarin. Don’t stop vitamin E cold turkey. Talk to your provider. Adjustments need to be managed.
If you’ve been taking vitamin E for years and feel fine, don’t assume you’re in the clear. The damage doesn’t always show up until it’s too late. The 2013 study found that patients with high vitamin E levels had bleeding events even when their INR was stable. That means your blood test might lie - but your body won’t.
What About Newer Blood Thinners?
Many people are switching from warfarin to DOACs like apixaban or rivaroxaban. Are they safer with vitamin E? Not necessarily. There’s less data, but the antiplatelet effect of vitamin E still exists. A 2023 European Society of Cardiology update didn’t rule out vitamin E risks with DOACs - it just said more research is needed. Until then, the same caution applies. Don’t assume switching drugs makes supplements safe.
Final Thought: It’s Not About Fear - It’s About Awareness
Vitamin E isn’t evil. It’s an antioxidant. It helps your cells. But when you’re on warfarin, your body is already walking a tightrope. Adding something that weakens platelets - even slightly - tips the balance. You don’t need to panic. You just need to know the numbers. Check your bottles. Talk to your provider. Don’t let a supplement you thought was harmless become the reason you end up in the ER.
Can I take vitamin E with warfarin if my INR is stable?
Stable INR doesn’t guarantee safety. Vitamin E affects platelets, not just clotting factors, so your INR may not reflect the increased bleeding risk. Some patients bleed even with normal INR levels. Avoid doses over 400 IU daily, and always inform your provider.
How much vitamin E is in a typical multivitamin?
Most multivitamins contain 100-134 IU of vitamin E. Check the label. If you’re also taking a separate vitamin E supplement, add the doses together. Staying under 400 IU total is the safest approach while on warfarin.
Do I need to stop vitamin E completely?
Not necessarily - but only if you’re taking 400 IU or less daily and your provider agrees. Many doctors recommend avoiding it entirely because of the risk and difficulty in monitoring. Food sources like nuts and seeds are fine - they won’t push you into dangerous territory.
Can genetic testing tell me if I’m at higher risk?
Yes. Variants in the CYP2C9 and VKORC1 genes make some people more sensitive to warfarin and its interactions. If you’ve had unexplained bleeding or unstable INR, ask your doctor about genetic testing. It can help personalize your care.
What should I do if I start bleeding while taking vitamin E and warfarin?
Stop taking vitamin E immediately and contact your healthcare provider. Signs include unusual bruising, nosebleeds, blood in urine or stool, severe headaches, or dizziness. These could signal internal bleeding. Don’t wait. Get checked right away.


12 Responses
Look, if you’re taking vitamin E over 400 IU while on warfarin, you’re basically playing Russian roulette with your internal organs. I’ve seen three patients bleed out from ‘harmless’ supplements. The fact that people still think ‘natural’ equals safe is why medicine is in crisis.
It’s not about the dose. It’s about the illusion of control. We think we can outsmart biology with pills and labels, but the body doesn’t care about your INR chart or your multivitamin’s fine print. It just responds. And when it does, it doesn’t ask permission.
My grandma took 800 IU of vitamin E for 12 years with warfarin. Never had a problem. Maybe your data is skewed. Or maybe you’re just scared of people being too healthy.
There’s a deeper truth here. We treat medicine like a spreadsheet. INR numbers. IU counts. Safe thresholds. But the body isn’t a machine. It’s a symphony. And vitamin E? It’s not a note. It’s a whisper that changes the whole harmony. You don’t hear it until the violin breaks.
Oh please. Big Pharma doesn’t want you taking vitamin E because it’s cheap and they can’t patent it. They make you pay $500 for a new blood thinner while your multivitamin costs $3. Wake up. The FDA is just a marketing arm for the drug companies.
While the empirical evidence presented in the original post is compelling and aligns with contemporary clinical guidelines, one must also consider the heterogeneity of patient populations and the limitations of observational studies. The correlation between serum vitamin E levels and bleeding events does not necessarily imply causation without controlled trials.
you know what else is dangerous? antibiotics. and coffee. and sunshine. everything is a threat if you wanna be paranoid. i take 600iu and my doc says i’m fine. maybe your doc is just scared of lawsuits. or worse - they don’t even know what they’re talking about.
They don’t tell you this but vitamin E is actually a cover for the government’s secret blood thinning program. They want you weak. That’s why they let supplements fly under the radar. You think they care if you bleed? No. They just want you dependent on their drugs. 400 IU? That’s the threshold they picked so you’d think you’re safe. It’s all a trap.
I’ve been on warfarin for 8 years. I take a multivitamin with 134 IU and a handful of almonds every day. My INR’s been stable. I never took a separate vitamin E pill. I’m not scared - I’m informed. Talk to your doctor. Know your numbers. But don’t let fear make you stop living. Food is fine. Supplements? Ask first.
Let me break this down for you real simple. You’re on warfarin. That means your body’s already working overtime just to not bleed to death. Now you add something that makes your platelets sluggish? You’re stacking the deck. Even if your INR looks good, your platelets are getting weaker. It’s like driving with worn brakes and thinking you’re fine because the speedometer says 55. You’re not. You’re one pothole away from disaster. Don’t gamble with your life. Skip the extra vitamin E. Your future self will thank you.
They say 400 IU is dangerous but what they dont say is that vitamin E is the only thing keeping my skin from falling off after chemo. and my cousin in delhi? she takes 1000iu and runs marathons. maybe its not the vitamin e - maybe its the fear they sell you. the system wants you scared so you take their pills. they dont want you strong. they want you dependent.
Stop.