Medication Interaction Checker
Check Your Medications
Results
Key Safety Information
Critical Risk Factors
- Patients over 65: 3x higher risk
- 5+ medications: 18x higher risk
- Women: 1.7x higher risk
When you take a statin for cholesterol or colchicine for gout, you probably don’t think about your muscles breaking down. But when two common medications mix, the result can be a silent, life-threatening crisis called rhabdomyolysis. It’s not rare. It’s not theoretical. It’s happening in hospitals right now - often because no one checked what else the patient was taking.
What Actually Happens When Muscles Break Down
Rhabdomyolysis isn’t just sore muscles after a hard workout. It’s when muscle cells rupture and spill their contents into your blood. The main danger? Myoglobin - a protein that turns urine dark brown, like cola. When too much of it floods your kidneys, it clogs the tiny filters. That’s how kidney failure starts. Up to half of people with severe rhabdomyolysis need dialysis. About 1 in 10 won’t survive if it’s not caught fast.
The telltale signs - muscle pain, weakness, and dark urine - only show up in about half the cases. The rest? They feel tired, nauseous, or have abdominal pain. Some even get a fever. By the time they go to the ER, it’s often too late. That’s why doctors miss it. And why you need to know the real red flags.
Statins Are the Biggest Culprit - But Only When Mixed
Statins like Lipitor and Zocor are the most common cause of drug-induced rhabdomyolysis. About 60% of all medication-related cases trace back to them. But here’s the catch: most statin users never have this problem. The risk skyrockets when they’re combined with other drugs that interfere with how the body breaks them down.
The problem is the liver enzyme CYP3A4. It’s like a garbage disposal for many medications. When another drug blocks it - like the antibiotic clarithromycin or the antifungal itraconazole - statins pile up in your system. The result? Muscle cells start dying. One study found that simvastatin plus clarithromycin increases rhabdomyolysis risk by nearly 19 times. That’s not a small bump. That’s a red alarm.
And it’s not just antibiotics. Fibrates, used for triglycerides, are even worse. Gemfibrozil mixed with simvastatin? Risk jumps 15 to 20 times. That combination should be avoided entirely. Yet it still happens. Why? Because many doctors don’t know the numbers. Or they assume the patient’s taking it safely.
Other Dangerous Mixes You Might Not Know About
Statins aren’t the only offenders. Colchicine, a common gout drug, is usually fine on its own. But when paired with clarithromycin or azole antifungals, it becomes a ticking time bomb. The European Medicines Agency warned in 2021: this combo increases risk by over 14 times. One patient on Reddit described it perfectly: “Added clarithromycin for a sinus infection. My urine turned dark within two days. CK hit 28,500. I was in the ICU.”
Then there’s erlotinib - a cancer drug for lung cancer. When taken with simvastatin, it can spike CK levels above 20,000 in just 72 hours. Oncologists focus on shrinking tumors. Muscle damage? Not always on their radar. A 2012 NIH case series documented this exact scenario. The patient needed dialysis. He survived. But he didn’t know the risk until it was too late.
Even propofol - the sedative used in surgery - can cause rhabdomyolysis in ICU patients. It’s rare, but deadly. When it happens, mortality hits 68%. Why? It shuts down energy production in muscle cells. Think of it like cutting the power to your muscles. They literally starve and die.

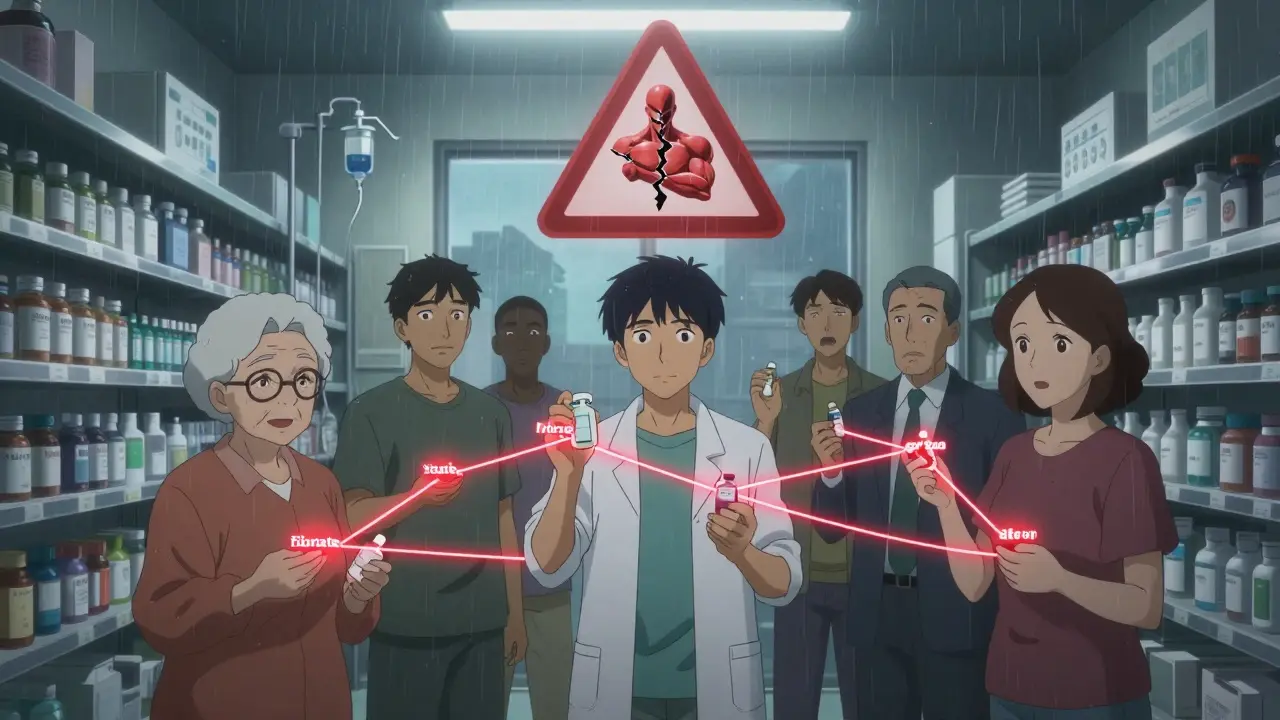
Who’s Most at Risk?
It’s not random. Certain people are far more likely to suffer this reaction.
- People over 65: Their kidneys don’t clear drugs as well. Risk is more than triple that of younger adults.
- Women: They’re 1.7 times more likely than men to develop drug-induced rhabdomyolysis.
- Those with kidney problems: If your eGFR is below 60, your risk jumps 4.5 times.
- Anyone taking five or more medications: Polypharmacy isn’t just a buzzword. It’s a major predictor. People on five+ drugs are nearly 18 times more likely to develop this condition.
There’s also a genetic factor. About 1 in 10 Europeans carry a gene variant called SLCO1B1*5. It makes them 4.5 times more sensitive to simvastatin’s muscle toxicity. Right now, no one routinely tests for it. But if you’ve had unexplained muscle pain on statins before, you might have it.
How It’s Diagnosed - And Why It’s Often Missed
The test is simple: a blood test for creatine kinase (CK). Normal levels are under 200 U/L. Anything over 1,000 U/L raises suspicion. Severe cases often hit 5,000 to 100,000 U/L. But here’s the problem: CK levels don’t rise immediately. It can take 12 to 24 hours after muscle damage starts. So if you feel sore after starting a new drug, and your CK is “only” 800, doctors might say, “It’s just exercise.”
And that’s where it gets dangerous. A 2022 study found that 92% of patients who later developed rhabdomyolysis had reported muscle aches or weakness - but their doctors didn’t connect the dots. Patients were told to “just rest.” Meanwhile, their muscles kept breaking down.
Urine color matters too. Dark, tea- or cola-colored urine is a classic sign. But not everyone notices. Some think it’s dehydration. Others assume it’s from food or supplements. Myoglobinuria is silent until it’s too late.
What Happens in the Hospital
If rhabdomyolysis is suspected, the clock starts ticking. First: stop the offending drug. Immediately. No delays.
Then: massive IV fluids. The goal? Flush out the toxins before they wreck your kidneys. The Cleveland Clinic protocol says: 3 liters of saline in the first 6 hours, then 1.5 liters per hour. Sometimes, they add sodium bicarbonate to keep urine pH above 6.5. That helps myoglobin dissolve instead of clumping up in the kidneys.
They also watch for dangerous electrolyte shifts:
- High potassium (hyperkalemia): Can cause heart rhythm problems. Happens in nearly 38% of severe cases.
- Low calcium (hypocalcemia): Can lead to muscle spasms or seizures.
- Compartment syndrome: Swelling in muscles cuts off blood flow. Needs emergency surgery.
Some patients need dialysis. Others need plasma exchange - especially if they’re on drugs like leflunomide, which sticks around in the body for weeks. One case from Massachusetts General Hospital involved a patient with CK over 50,000 U/L. Plasma exchange saved his kidneys.
Recovery - And the Hidden Long-Term Cost
Surviving rhabdomyolysis doesn’t mean you’re back to normal. In a 10-year Mayo Clinic study, nearly half of survivors still had muscle weakness six months later. Full recovery without kidney damage takes about 3 months. With dialysis? More than 6 months.
And the emotional toll? Many patients feel betrayed. “My doctor never warned me,” is a common refrain on patient forums. One man, after his 3-day dialysis stint, said: “I was told statins were safe. Now I can’t even climb stairs without pain.”
There’s also financial damage. In the U.S., the average hospital bill for drug-induced rhabdomyolysis is nearly $29,000. That’s not insurance. That’s out-of-pocket risk for many.
How to Protect Yourself
You can’t control everything. But you can control what you ask.
Before starting any new medication - even an antibiotic or antifungal - ask:
- “Could this interact with any of my other drugs?”
- “Is there a risk of muscle damage?”
- “Should I stop my statin while taking this?”
Keep a list of everything you take - including supplements and OTC meds. Bring it to every appointment. Don’t assume your pharmacist or doctor knows your full history.
If you start feeling unusual muscle pain, weakness, or notice dark urine after a new drug, go to urgent care. Don’t wait. Don’t assume it’s “just soreness.” Get a CK test. It takes 15 minutes. It could save your kidneys.
And if you’re on statins, know your numbers. Your doctor should check your CK before you start - and again if you’re added to a new medication. If they don’t, ask. You’re not being difficult. You’re being smart.
What’s Changing - And What’s Not
Regulators are catching up. The EMA now requires statin labels to list specific drug interactions. The FDA’s Sentinel system tracks these cases in real time. In 2020, they saw a spike in rhabdomyolysis reports after remdesivir was used for COVID - a sign that even new drugs carry hidden risks.
But the real problem isn’t the drugs. It’s the system. Doctors are rushed. Pharmacies don’t always flag interactions. Patients don’t know to ask. And muscle pain? It’s dismissed as aging, exercise, or stress.
Until we treat medication interactions like the emergencies they are - until we stop assuming safety - this will keep happening. Because rhabdomyolysis doesn’t care if you’re healthy, young, or took your meds “as directed.” It only cares if two drugs met in your bloodstream.
Know your meds. Know your risks. Speak up. Your muscles - and your kidneys - depend on it.


9 Responses
Statin + clarithromycin = bad combo. I work in a pharmacy in Delhi, and we see this all the time. Elderly patients on statins get antibiotics for colds and never tell their doctor. One guy ended up in ICU. Just ask your doc before taking anything new. Simple.
man i had no idea muscle breakdown could be this sneaky. i thought dark urine was just from drinking too much protein shake or being dehydrated 😅
now i’m gonna check all my meds before i take anything else. this post saved my life probably.
Oh please. You’re acting like this is some groundbreaking revelation. Every pharmacist in America knows this. The real problem? Doctors are lazy, patients are dumb, and the FDA is asleep at the wheel. You think a ‘warning label’ stops someone from popping a statin with an antibiotic? HA. People take Tylenol with alcohol and don’t die? Nah. This is just fearmongering dressed up as ‘education.’
And don’t even get me started on ‘genetic testing’ - you want to spend $500 to find out you’re sensitive to simvastatin? Just don’t take it. Duh.
Good post. Important stuff.
But please, if you’re on statins and get a new script - even for a sinus infection - ask about muscle risk. No shame in asking. You’re not bothering anyone.
It is unconscionable, utterly irresponsible, and frankly criminal, that physicians continue to prescribe these dangerous combinations without mandatory interaction screening. The healthcare system is not merely broken-it is actively predatory toward the elderly, the polypharmacy-dependent, and the medically vulnerable. This is not negligence; it is systemic malpractice. And yet, we are told to ‘speak up’? As if patient advocacy is a substitute for professional accountability.
Wow. So the solution is… to read the label? Groundbreaking. I bet if we all just remembered to breathe, we’d stop getting cancer too. 🙃
my doc never told me about the clarithromycin thing… i took it last year and got super sore legs. thought it was just from mowing the lawn. ugh. i’ll bring my med list next time. sorry for the typos, typing on phone.
bro i’ve been on simvastatin for 5 years and just got azithromycin for a cough last month… i’m checking my pee every day now 😅
also, my grandma died from kidney thing after taking colchicine + antibiotic… so this hits hard.
Just stopped my statin for a week while on antibiotics. Worth the extra 7 days of cholesterol anxiety. Better safe than ICU.