Medication-Induced IIH Risk Checker
Check Your Risk
This tool helps identify if your symptoms might be related to medication-induced pseudotumor cerebri (IIH). It's not a diagnosis, but can help you determine if you should see a doctor immediately.
Risk Assessment
Your risk score:
Important disclaimer: This tool is for educational purposes only. It is not a substitute for professional medical advice. If you experience severe headaches or vision changes, contact your doctor immediately.
When you start a new medication for acne, rosacea, or another condition, you expect relief-not a pounding headache that won’t quit, or moments when your vision goes gray for seconds at a time. But for some people, common prescriptions can trigger a rare but dangerous condition called pseudotumor cerebri, also known as medication-induced idiopathic intracranial hypertension (IIH). It’s not a brain tumor. But it acts like one: pressure builds inside the skull, squeezing the optic nerves and causing symptoms that can lead to permanent vision loss if ignored.
What Exactly Is Pseudotumor Cerebri?
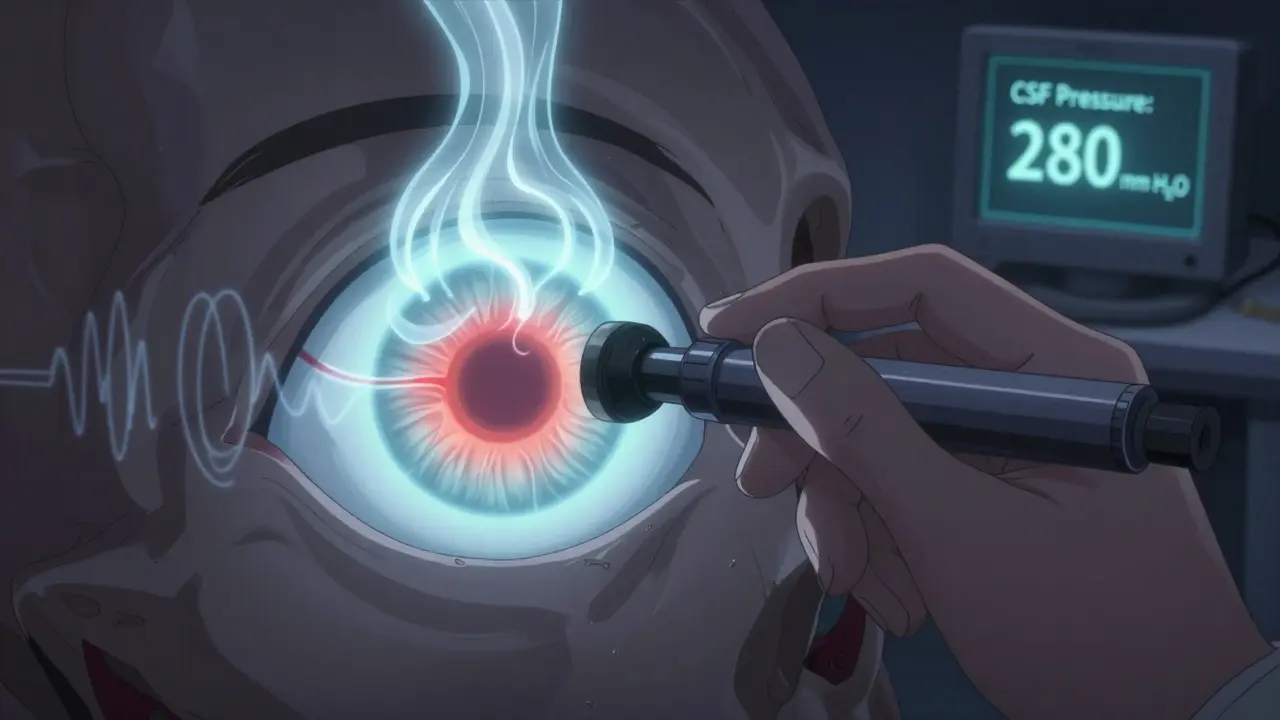
Pseudotumor cerebri means "false brain tumor." It’s when the pressure of the fluid surrounding your brain and spinal cord-cerebrospinal fluid (CSF)-rises without any tumor, infection, or blockage. Normal CSF pressure is between 70 and 180 mm H₂O. In pseudotumor cerebri, it spikes above 250 mm H₂O. That’s like wearing a helmet that’s too tight, day and night. The brain doesn’t have room to expand, so it presses against nerves, especially the optic nerve behind the eye.
Most cases are called "idiopathic," meaning doctors don’t know why it happens. But about 10-15% of cases are directly caused by medications. These aren’t rare side effects-they’re well-documented, predictable reactions that often get missed because they look like migraines or sinus infections.
Which Medications Trigger It?
Not every drug causes this. But certain ones have a clear link. The most common culprits include:
- Minocycline (a tetracycline antibiotic): Used for acne and rosacea. It’s the #1 medication linked to IIH in young adults. One case occurs for every 7,500 prescriptions.
- Isotretinoin (Accutane): A powerful acne treatment. Symptoms can appear within 4-8 weeks, and vision loss can develop faster than with any other trigger.
- Corticosteroid withdrawal: Stopping prednisone or similar drugs after long-term use can cause a sudden spike in pressure. This form has the highest risk of permanent vision damage-up to 18% of cases.
- Growth hormone therapy: Mostly affects children. In 22% of pediatric cases, vision changes happen before headaches even start.
- Excess vitamin A: High-dose supplements or foods rich in retinol can trigger it, especially when combined with isotretinoin.
Here’s the scary part: using two of these together-like minocycline and isotretinoin-multiplies your risk by 7.3 times. That’s not theoretical. A 2022 study of 142 patients found this combo was behind many of the worst cases.
What Do the Symptoms Feel Like?
People often mistake these signs for stress, migraines, or allergies. But there are clues that point to something more serious:
- Severe headaches: Reported in 92-95% of cases. They’re worse when lying down, bending over, or straining. Many describe them as "thunderclap"-sudden, intense, and unlike anything they’ve felt before.
- Transient visual obscurations: Your vision goes gray, blurry, or dark for 5-15 seconds. It happens multiple times a day, often when standing up or coughing. Over 70% of patients experience this.
- Pulsatile tinnitus: You hear your own heartbeat in your ears, especially when lying still.
- Double vision or blurred vision: Caused by pressure on the nerves that control eye movement.
- Permanent vision loss: If untreated, 5-10% of patients lose peripheral vision permanently. In corticosteroid withdrawal cases, that number jumps to 18%.
One patient on a rare disease forum described it this way: "I kept thinking I was just tired. Then I started seeing gray spots every time I stood up. By the time I saw a neurologist, I’d lost 30% of my side vision. I thought I was going blind. I wasn’t."
Why Is It So Often Missed?
Doctors aren’t negligent-they’re overwhelmed. A 2022 study found that 65-70% of primary care physicians first diagnose medication-induced IIH as migraine (33%) or sinusitis (41%). The delay? On average, 4 to 12 weeks. That’s enough time for irreversible damage.
Why? Because the symptoms mimic common problems. Headaches are everywhere. Vision changes? Maybe it’s eye strain from screens. But if you’re on minocycline or isotretinoin and suddenly get daily headaches that get worse lying down? That’s not normal. That’s a red flag.
Even specialists can miss it. One patient, "AcneWarrior," shared on HealthUnlocked: "My ophthalmologist missed the papilledema for three months. I stopped Accutane right away, but it was too late. I have permanent blind spots now."
How Is It Diagnosed?
If you’re on a high-risk medication and have these symptoms, you need a specific diagnostic path:
- Stop the suspected medication immediately. Don’t wait for test results. This alone can stop progression.
- Lumbar puncture (spinal tap). This is the gold standard. It measures CSF pressure directly. If it’s above 250 mm H₂O, you have IIH.
- Eye exams. An ophthalmologist will check for papilledema-swelling of the optic nerve. This is visible through an ophthalmoscope.
- Visual field testing. A Humphrey perimetry test detects early blind spots, often in the upper nasal field, before you even notice them.
- Optical coherence tomography (OCT). This scan measures the thickness of the retinal nerve fiber layer. A spike of 15-20 microns in the first week is a telltale sign.
Crucially, MRI or CT scans are often normal in pseudotumor cerebri. That’s why it’s called a "false" tumor. If your scan is clean but you still have symptoms and high CSF pressure? That’s the diagnosis.
What Happens After Diagnosis?
Once the trigger is removed, many people improve. But recovery isn’t instant.
- Headaches often take 4-12 weeks to fade, even after stopping the drug.
- Vision recovery depends on how long pressure was high. Some regain full sight. Others have permanent damage.
- Medications like acetazolamide (Diamox) or the newer venglustat (approved in 2023) help reduce CSF production and lower pressure.
- In severe cases, a shunt may be placed to drain excess fluid from the brain.
One Reddit user, u/MinocyclineSurvivor, wrote: "I stopped minocycline and took acetazolamide for 6 weeks. My vision came back completely. But the headaches? Took four months to disappear. I wish I’d known sooner."

Who’s at Risk?
It’s not just about the drug-it’s about who’s taking it.
- Minocycline users: Mostly young women aged 15-25. Off-label use for rosacea has made this group grow rapidly since 2015.
- Isotretinoin users: Teens and young adults with severe acne. FDA and EMA now require monthly eye exams during treatment.
- Children on growth hormone: Vision loss can happen before headaches appear. Regular fundoscopic checks every 3 months are essential.
- People stopping steroids: Risk is highest in the first 1-3 weeks after discontinuation.
Obesity is a major risk factor in idiopathic IIH-but not in medication-induced cases. That’s why it can strike men, children, and slim adults too.
Can It Be Prevented?
Yes-if you know the signs and act fast.
- If you’re prescribed minocycline, isotretinoin, or corticosteroids, ask your doctor: "Could this cause increased pressure in my head?"
- Know your symptoms. If you get new, severe headaches that worsen when lying down, don’t ignore them.
- Report any vision changes immediately-even if they’re brief.
- If you’re on two high-risk drugs (like minocycline + isotretinoin), insist on baseline eye exams before starting.
- Keep a symptom diary: When did the headache start? How bad is it? When does your vision blur? This helps doctors connect the dots.
Since the EU started requiring monthly eye checks for isotretinoin users, permanent vision loss dropped from 12% to 4.7%. That’s proof that awareness saves sight.
What’s Next?
Researchers are working on better tools. A 2023 study at Johns Hopkins found three specific inflammatory markers that appear only in medication-induced IIH-not in idiopathic cases. That could lead to a blood test that confirms the cause within hours.
The IIH Registry Project, launched in January 2023, is tracking 500 patients to map out exactly how long after taking a drug symptoms appear. That will help doctors spot patterns faster.
But right now, the best defense is knowledge. If you’re on a medication linked to this condition, and you start having headaches that feel "off," don’t wait. Don’t assume it’s stress. Don’t take another painkiller and hope it goes away. Get checked. Your vision might depend on it.


10 Responses
so i was on minocycline for 6 months for my acne and never thought twice until i started seeing gray spots when i stood up... thought i was just dizzy from coffee. turned out my optic nerve was swollen like a balloon. docs said if i’d waited another week i might’ve lost peripheral vision for good. now i’m on antibiotics that don’t try to kill my eyes. fyi: if you’re on this stuff and your head feels like it’s in a vice? stop. go. now.
Thank you for sharing this vital information. As a healthcare professional, I cannot emphasize enough how frequently this condition is misdiagnosed. The symptoms mimic common ailments, and without a high index of suspicion, especially in young women on acne medications, irreversible damage can occur. Please, if you are prescribed isotretinoin or minocycline, request a baseline fundoscopic exam. Prevention is far kinder than recovery.
Let’s be real-this isn’t some mysterious medical miracle. Big Pharma knows these drugs cause intracranial pressure. They just don’t care because lawsuits are cheaper than reform. And doctors? They’re paid to prescribe, not to think. You think Accutane’s warning label is clear? It’s buried in 12-point font next to ‘may cause mild nausea.’ Meanwhile, kids are going blind and the FDA’s still approving new formulations. Wake up. This is capitalism in medicine.
To anyone reading this: if you’re on minocycline or isotretinoin and have new headaches or vision changes-don’t wait. Don’t second-guess yourself. Go to the ER or see a neuro-ophthalmologist. You’re not overreacting. Your body is screaming. I’ve seen patients recover fully when they acted fast. You deserve to keep your sight. Please, don’t be like me-I waited three weeks. You don’t have to.
It’s fascinating how modern medicine has become a high-stakes game of Russian roulette with pharmaceuticals. We’ve replaced natural remedies with synthetic compounds that subtly erode our neurological integrity-while marketing them as ‘safe’ and ‘routine.’ The fact that this condition is so rarely discussed speaks volumes about our systemic failure to prioritize long-term health over short-term cosmetic outcomes. The real pseudotumor isn’t in the skull-it’s in the medical-industrial complex.
honestly i thought i was just stressed out until i started hearing my heartbeat in my ears while trying to sleep... then i saw a gray curtain every time i stood up. i went to my derm and they just gave me more ibuprofen 😭 turned out i had papilledema. now i'm off everything and seeing a neurologist. if you're on acne meds and your head feels like it's gonna explode-listen to your body. not the ads. 🙏
Of course this happens. Every time a drug gets approved for ‘cosmetic’ use, people treat it like a vitamin. Minocycline for acne? Isotretinoin for ‘a few pimples’? You’re not treating acne-you’re gambling with your optic nerves. And don’t get me started on how doctors hand these out like candy. This isn’t science. It’s negligence dressed up as skincare.
i had this. stopped the medicine, took the pills they gave me, and it took forever to feel normal again. but i didn't lose my sight. if you're reading this and you're on one of those meds and your head hurts all the time? don't wait. go get it checked. it's not just a headache.
bro i was on minocycline and isotretinoin together for 2 months... thought my brain was melting. headaches so bad i cried. doc said it was 'just acne stress.' i went to another doc and they did the spinal tap. pressure was 310. i was terrified. now i'm off both and my vision is back. don't let anyone tell you it's not real. it is.
Some people think beauty is worth a blind spot. I think they’re wrong. You don’t need flawless skin to be worthy. But you do need your eyes to see the people you love. If you’re taking these meds for vanity-ask yourself: is this worth losing the ability to see your child’s first smile? Your partner’s face? Your own reflection? I’m not judging. I’m warning.