When fluid builds up in your tissues, you notice swelling, a condition called oedema is the accumulation of excess fluid in the interstitial spaces, often visible as puffiness or swelling in the legs, hands, face, or abdomen. While many think of heart or kidney problems first, a surprising number of autoimmune disorders are diseases where the immune system mistakenly attacks the body’s own tissues, causing chronic inflammation and a cascade of secondary effects. Understanding how these two issues intersect can help you spot warning signs early, talk to your doctor with the right questions, and manage symptoms more effectively.
How Oedema Forms in the Body
Fluid normally circulates through blood vessels, the interstitial space, and the lymphatic system. Four main forces keep that balance in check:
- Hydrostatic pressure pushing fluid out of capillaries.
- Oncotic pressure pulling fluid back in, mainly from albumin.
- Capillary permeability, which determines how easily fluid leaks.
- Lymphatic drainage, the cleanup crew that returns excess fluid to circulation.
When any of these factors get thrown off-by heart failure, kidney disease, low protein, or inflammation-fluid pools and oedema appears.
Autoimmune Disorders: A Quick Overview
Autoimmune conditions cover a wide spectrum, from organ‑specific attacks (like thyroiditis) to systemic assaults (like lupus). They share two core features:
- Persistent inflammation driven by cytokines such as TNF‑α, IL‑6, and interferon‑γ.
- Altered blood‑vessel and lymphatic function, which can raise vascular permeability and hinder drainage.
These mechanisms set the stage for oedema, especially when the disease targets organs that regulate fluid balance.
Diseases Most Frequently Linked to Oedema
Not every autoimmune disease causes swelling, but several do, often in characteristic patterns.
| Disease | Typical Edema Location | Prevalence (US) | Key Lab Marker |
|---|---|---|---|
| Rheumatoid arthritis | Hands, feet, ankles | ~1.3% | RF & anti‑CCP antibodies |
| Systemic lupus erythematosus | Facial (malar), peritoneal, pleural | ~0.05% | ANA, anti‑dsDNA |
| Hashimoto thyroiditis | Periorbital, myxedema (non‑pitting) | ~5% women | Elevated TSH, anti‑TPO |
| Celiac disease | Legs, abdomen (due to protein loss) | ~1% | tTG‑IgA, EMA |
Rheumatoid Arthritis and Swelling
Rheumatoid arthritis is a chronic inflammatory joint disease that primarily attacks the synovium, leading to pain, stiffness, and joint deformity. The inflammation releases cytokines that make capillaries leaky, so fluid seeps into surrounding tissues. This usually shows up as pitting edema in the hands, feet, and ankles. If you notice sudden hand swelling accompanied by morning stiffness, it could be a red flag.
Lupus‑Related Fluid Build‑Up
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease that can affect skin, kidneys, heart, lungs, and blood vessels. Kidney involvement (lupus nephritis) reduces the organ's ability to excrete sodium and water, leading to generalized edema. Additionally, inflammation of the pleura or peritoneum produces fluid‑filled cavities (pleural effusion, ascites), which feel like swelling in the chest or abdomen.
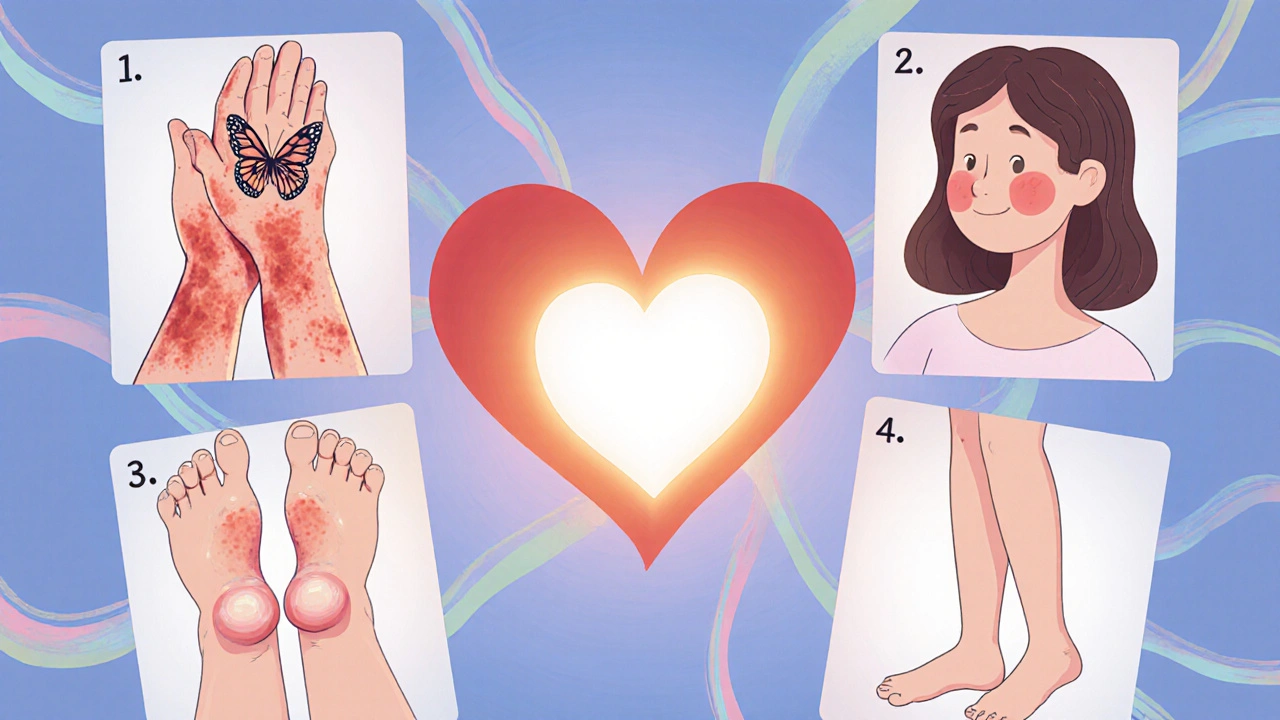
Hashimoto Thyroiditis and Myxedema
Hashimoto thyroiditis is the most common cause of hypothyroidism, where autoantibodies destroy thyroid cells. Low thyroid hormone slows metabolism, leading to mucopolysaccharide buildup in the skin-a non‑pitting form of edema called myxedema. You’ll often see puffiness around the eyes and a thickened, waxy skin texture.
Celiac Disease and Protein Loss
Celiac disease is an immune‑mediated reaction to gluten that damages the small‑intestinal lining. Damage impairs protein absorption, lowering serum albumin and reducing oncotic pressure. The resulting fluid shift tends to collect in the lower limbs, especially after prolonged standing.
Underlying Biological Mechanisms
The bridge between these diseases and edema can be boiled down to three biological pathways:
- Increased vascular permeability: Cytokines such as IL‑1β and TNF‑α open tight junctions between endothelial cells, letting plasma leak into tissues.
- Lymphatic dysfunction: Chronic inflammation can scar or compress lymphatic vessels, hampering fluid return. The lymphatic system is a network of vessels and nodes that drains interstitial fluid back into the bloodstream.
- Renal involvement: Autoimmune attacks on the kidneys (as seen in lupus nephritis) diminish filtration, causing sodium and water retention. The kidneys’ renal function is crucial for maintaining fluid and electrolyte balance.
Diagnosing Oedema Linked to Autoimmunity
Because swelling can stem from many sources, doctors follow a step‑by‑step approach:
- History and physical exam - note swelling pattern, onset, associated joint pain, skin changes, or organ‑specific symptoms.
- Blood tests - complete blood count, ESR/CRP for inflammation, disease‑specific antibodies (RF, anti‑CCP, ANA, anti‑TPO, tTG‑IgA).
- Urine analysis - proteinuria signals kidney involvement, especially in lupus.
- Imaging - ultrasound for joint effusion, echocardiogram if heart failure is suspected, and Doppler studies to rule out venous obstruction.
When labs point toward an autoimmune process, rheumatologists or endocrinologists take the lead.

Managing the Swelling
Effective treatment targets both the underlying immune disease and the fluid retention itself.
Control the Autoimmune Activity
- DMARDs (disease‑modifying antirheumatic drugs) for rheumatoid arthritis - methotrexate, sulfasalazine, or biologics like adalimumab.
- Immunosuppressants for lupus - mycophenolate, azathioprine, or low‑dose steroids during flares.
- Thyroid hormone replacement for Hashimoto - levothyroxine titrated to normalize TSH.
- Strict gluten‑free diet for celiac disease to restore gut integrity and protein absorption.
Direct Edema Relief
- Compression stockings for lower‑leg swelling.
- Elevating affected limbs above heart level for 15‑20 minutes, several times a day.
- Low‑salt diet to reduce fluid retention.
- Diuretics (e.g., furosemide) when kidney‑related fluid overload is present - always under physician guidance.
- Skin‑care for myxedema - moisturizing creams and gentle massage to improve lymphatic flow.
Regular monitoring of disease activity scores ( DAS28 for RA, SLEDAI for lupus) helps adjust therapy before swelling worsens.
When to Seek Immediate Care
If you notice any of these red flags, call your doctor or go to the emergency department:
- Sudden, severe swelling in the face or throat (possible angio‑edema).
- Shortness of breath accompanied by chest or abdominal swelling (could signal pleural effusion or ascites).
- Rapid weight gain (>5% in a week) with generalized puffiness.
- Fever, joint pain, and swelling that develop together - may indicate a flare.
Key Takeaways
- Oedema often signals an underlying autoimmune condition, especially if it appears with joint pain or skin changes.
- Rheumatoid arthritis, lupus, Hashimoto thyroiditis, and celiac disease are the most common culprits.
- Inflammation, lymphatic blockage, and kidney involvement are the three main pathways linking autoimmunity to swelling.
- Accurate diagnosis combines history, targeted labs, and imaging; early specialist referral improves outcomes.
- Treatment combines disease‑specific drugs with practical edema‑reduction strategies like elevation, compression, and diet.
Frequently Asked Questions
Can edema be the first sign of an autoimmune disease?
Yes. In many cases, swelling appears before classic joint pain or fatigue. For example, myxedema can precede overt hypothyroid symptoms, and peripheral edema may show up before lupus patients develop a rash or kidney issues.
Is all edema painful?
Not always. Pitting edema from heart or kidney problems often feels heavy but not sharp. Inflammatory edema, as seen in rheumatoid arthritis, can be tender because the underlying joint tissue is inflamed.
Do over‑the‑counter diuretics help?
OTC diuretics are weak and not recommended for disease‑related edema. Prescription diuretics, prescribed after labs confirm fluid overload, are far more effective and safer.
How does a gluten‑free diet affect leg swelling in celiac disease?
Removing gluten heals the intestinal villi, improves protein absorption, restores albumin levels, and consequently raises oncotic pressure. Most patients notice reduced leg edema within weeks of strict adherence.
Should I avoid all salty foods if I have autoimmune‑related edema?
A low‑salt diet (under 2g sodium per day) is advisable, especially if you have kidney involvement or are on diuretics. However, moderate salt isn’t harmful for isolated inflammatory edema; focus on overall balanced nutrition.


12 Responses
Wow, the way edema intertwines with autoimmune havoc is like a drama unfolding in your own body! First, remember that fluid balance is governed by hydrostatic and oncotic pressures, plus the lymphatic sweep-when any of these go haywire, swelling skyrockets. In rheumatoid arthritis, the synovial inflammation releases TNF‑α and IL‑1β, punching holes in capillary walls and letting plasma seep into the hands and feet. Lupus takes it a step further; renal involvement drops the kidneys’ filtering power, so sodium and water hang around like unwanted guests. Hashimoto’s thyroiditis slows metabolism, leading to mucopolysaccharide buildup, which you’ll spot as non‑pitting myxedema around the eyes. Celiac disease robs you of protein, dragging down albumin and pulling fluid into the lower legs. The common thread is cytokine‑driven vascular permeability and often a compromised lymphatic return. That’s why a simple leg raise can feel like a rescue mission for your interstitium. Compression stockings act as a mechanical hug, nudging fluid back toward the heart. Low‑salt diets cut the sodium‑water duet, and diuretics are the pharmacologic fire‑fighters when the kidneys are overwhelmed. Keep an eye on disease activity scores-DAS28 for RA or SLEDAI for lupus-to adjust therapy before the swelling worsens. Regular labs, especially ESR/CRP and disease‑specific antibodies, give you the early warning lights. Don’t forget to ask your rheumatologist about biologics that specifically target TNF‑α if standard DMARDs fall short. And if you ever feel that tightness in your throat or sudden facial puffiness, treat it as an emergency-angio‑edema can be life‑threatening. Finally, remember that lifestyle tweaks like staying hydrated, gentle exercise, and a balanced gluten‑free or iodine‑rich diet can keep the fluid tides in check. Stay proactive, stay informed, and you’ll turn the tide on edema before it decides to crash your day!
Thanks for the detailed overview, Jeff. The link between cytokine‑driven permeability and lymphatic overload is especially important for patients who think swelling is just “water weight.” In practice, checking albumin levels early can help differentiate protein‑losing states from pure inflammatory edema. Also, simple home measures-elevating legs for 15 minutes three times a day-often reduce pitting edema noticeably. It’s useful to pair these steps with regular monitoring of disease‑specific markers.
Honestly, the article-while thorough-misses the obvious: most clinicians already know that TNF‑α blows up capillary walls, and they’re not going to reinvent the wheel, right?; the real problem is that patients often ignore basic sodium restriction, yet they keep blaming “autoimmune flare” for every puff!; plus, the suggestion to “just elevate limbs” sounds like a lazy Band‑Aid, not a comprehensive treatment plan; and don’t even get me started on the vague “low‑salt diet” advice-how low is low?; we need concrete numbers, not vague recommendations, otherwise it’s just noise.
If you ignore the swelling, youre just asking for trouble.
It's interesting how our bodies whisper warnings through fluid shifts-like a river finding its course. Sometimes the swelling is just the system's way of saying "slow down" and rethink our habits :) Embracing gentle movement and mindful breathing can actually aid lymphatic flow, turning that whisper into a smoother current. Staying attuned to these signals feels like a quiet meditation on health.
Oh sure, because "gentle movement" will magically unclog your lymphatics-next you'll tell me yoga mats are the cure for lupus nephritis. Let's be real: the pathophysiology involves cytokine cascades, endothelial dysfunction, and renal hemodynamics, not some mystical Chi flow. If you want to talk shop, bring up the NF‑κB signaling pathway and the role of selective JAK inhibitors, not "feel‑good vibes". Also, dropping the "gluten‑free" bomb doesn’t fix albumin loss unless you address villous atrophy head‑on. So spare us the airy‑fairy remedies and stick to evidence‑based protocols, ok?
I appreciate the thoroughness of the information presented; it offers a clear roadmap for those navigating complex autoimmune conditions.
Thanks, Sinead. I agree that having a step‑by‑step diagnostic approach can really demystify the process for patients. It’s also helpful to know which labs are most predictive of early edema in the context of autoimmune disease. I’ve found that adding a basic metabolic panel to the workup often catches subtle electrolyte shifts before they become symptomatic.
Yeah, the basic metabolic panel is key-i even tripped over a missing potassium result once and the patient ended up with foot swelling. also, i noticed that sometimes the doc forgets to order a urine protein check, which is a big miss. just a heads up for anyone reading.
Mark makes a solid point about urine protein; microalbuminuria can be the silent harbinger of lupus nephritis before overt edema appears. Incorporating a spot urine protein‑to‑creatinine ratio into routine follow‑ups is a low‑cost way to catch that early. Moreover, educating patients on self‑monitoring for sudden weight changes can prompt timely interventions. A collaborative approach between rheumatology and nephrology truly optimizes outcomes.
Great thread, folks! I love how we’re mixing science with real‑world tips. Remember, staying hydrated (but not over‑hydrated) keeps your kidneys happy, and a splash of colorful fruits can make low‑salt meals exciting. Keep sharing what works for you-together we make the best health toolbox.
Totally agree, Taylor. Simple steps make a big difference.