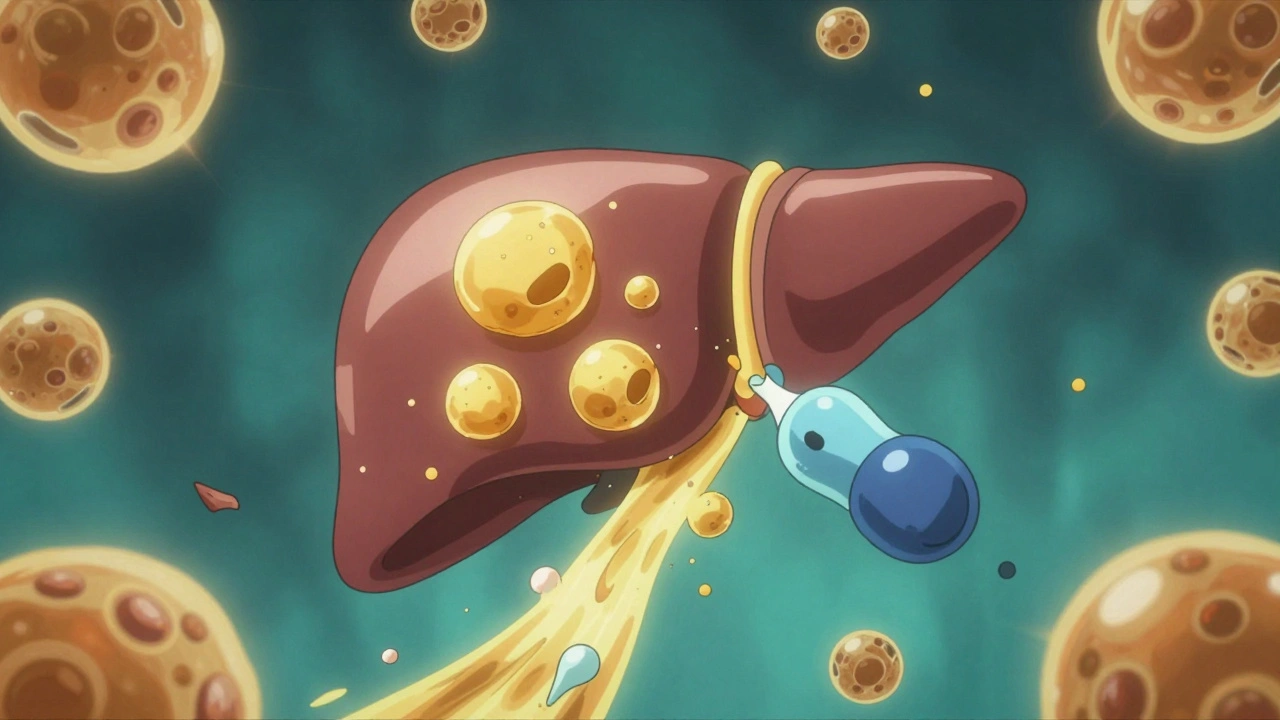
More than one in four adults worldwide has fat building up in their liver - not from drinking alcohol, but from metabolic issues like obesity, diabetes, or high blood pressure. This isn’t just a minor glitch in your body. Left unchecked, it can lead to inflammation, scarring, and even liver failure. The condition used to be called NAFLD, but since 2023, experts call it MASLD - Metabolic Dysfunction-Associated Steatotic Liver Disease. The name change matters because it means diagnosis isn’t about ruling things out anymore. It’s about finding the metabolic problems that are actually causing the damage.
Why Your Liver Gets Fat
Your liver doesn’t store fat for fun. When your body’s metabolism goes off track, fat starts pooling there. About 59% of that fat comes from your belly fat breaking down and sending free fatty acids straight to your liver. Another 26% is made inside your liver from excess sugar and carbs you eat. The rest comes from your diet. Meanwhile, your liver’s ability to burn fat or ship it out drops. It’s like a clogged drain with the tap still running.Insulin resistance is the main culprit. When your fat cells can’t respond to insulin properly, they leak fat into your bloodstream. That fat floods your liver. At the same time, your liver starts making more fat from sugar - a process called de novo lipogenesis. Inflammation follows. Immune cells get activated. Scarring begins. This isn’t just fatty liver anymore. It’s MASH - Metabolic Dysfunction-Associated Steatohepatitis - and it’s on its way to cirrhosis in up to 30% of cases over 10 to 15 years.
Weight Loss Isn’t Optional - It’s the Treatment
The best thing you can do for MASLD isn’t a pill. It’s losing weight. Not a little. Not a little bit. Enough to actually change your liver.Studies show that losing just 5 to 7% of your body weight reduces fat in your liver. But if you want to reverse inflammation and scarring - the real danger signs - you need to hit 10% or more. The Look AHEAD trial found that people who lost 10% of their weight cut their risk of developing MASH by 90%. That’s not a small win. That’s life-changing.
How does it work? When you lose weight, your fat cells stop leaking fatty acids like a broken pipe. That cuts the main source of liver fat by 30 to 40%. Your liver also slows down its own fat production by 25 to 35%. And it starts burning fat again - better than it has in years. Magnetic resonance scans show liver fat dropping visibly within months of sustained weight loss.
The European Association for the Study of the Liver recommends a 7 to 10% weight loss goal over six to twelve months. That means about 150 to 300 minutes of brisk walking or cycling each week, and cutting daily calories to between 1,200 and 1,800, depending on your size. No magic diets. No detoxes. Just steady, real weight loss.
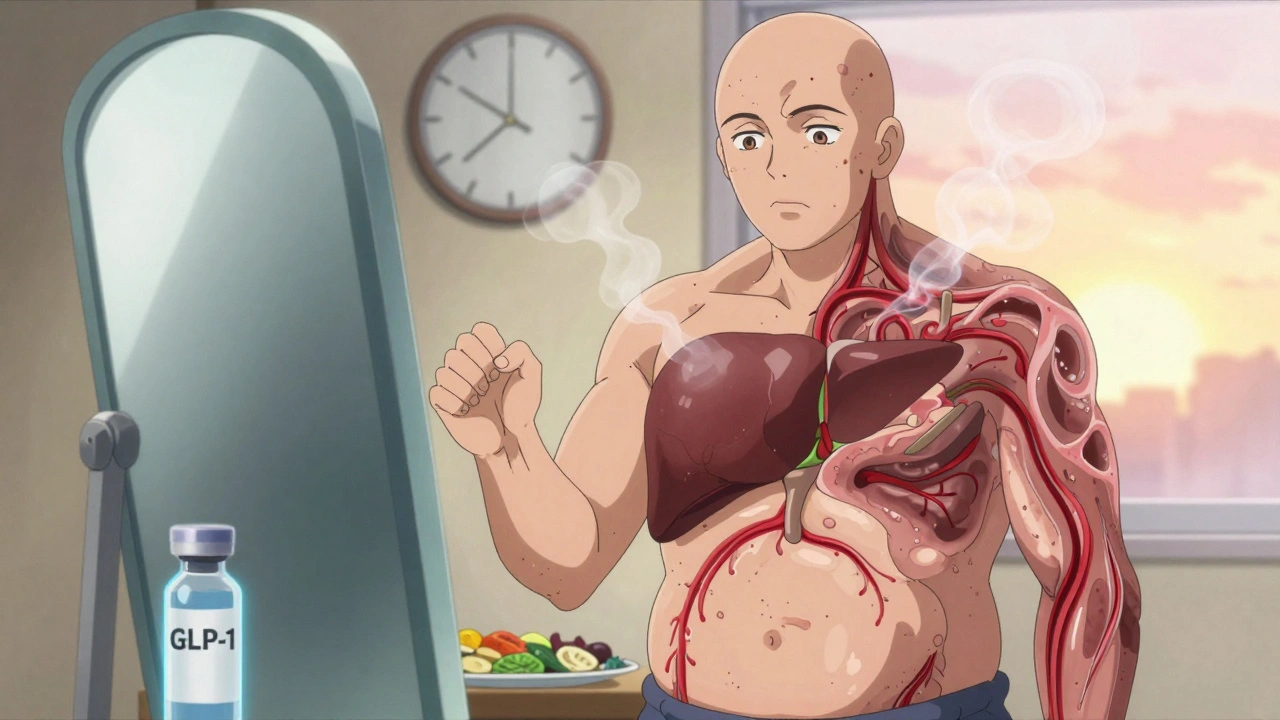
GLP-1 Drugs: A Game Changer for Many
For many people, losing 10% of their body weight through diet and exercise alone is incredibly hard. That’s where GLP-1 receptor agonists come in. These drugs - like semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda) - were first designed for diabetes. But they turned out to be powerful weight-loss tools.Semaglutide, at the 2.4 mg weekly dose, helped people lose an average of 15% of their body weight in clinical trials. In one study, 55% of MASLD patients saw their liver fat cut in half. Liraglutide helped 39% of patients reverse MASH - compared to just 17% on placebo.
How do they work? GLP-1 drugs make you feel full faster. They slow down your stomach. They reduce hunger signals to your brain. But they also act directly on your liver. They improve insulin sensitivity in fat tissue, so less fat leaks into the liver. They turn down fat-making machinery inside liver cells. And they calm inflammation by blocking key inflammatory pathways.
The REGENERATE trial showed that semaglutide at 1.0 mg weekly led to MASH resolution in 52% of patients after 72 weeks - nearly double the placebo rate. These aren’t just numbers. These are real people with less liver damage.
The Real-World Struggle
But here’s the truth: not everyone sticks with it.On patient forums, 68% of people say they can’t keep off 10% of their weight after a year. More than 40% regain half of it within two years. And GLP-1 drugs? Side effects are real. Nausea, vomiting, and stomach pain are common. On Reddit’s fatty liver community, 76% of users reported nausea. About one in three quit within six months because they couldn’t tolerate it.
Still, success stories exist. One patient on HealthUnlocked lost 12.3% of his weight over nine months on semaglutide. His FibroScan showed liver fat dropping from 328 to 245 dB/m - a clear sign of healing. The key? He didn’t just take the drug. He worked with a dietitian, stuck to a Mediterranean-style diet, and cut fructose to under 25 grams a day.
When GLP-1 drugs are paired with structured support, adherence jumps from 42% to 65%. That’s the difference between giving up and getting better.
What Doctors Do Now
Top clinics like Duke’s MASLD program don’t just hand out prescriptions. They start with tests. FibroScan to measure liver stiffness. MRI-PDFF to see exactly how much fat is there. Blood tests to calculate FIB-4 - a simple score that predicts scarring risk.Then they build a plan. First three months: weekly visits with a dietitian. Focus on whole foods, no sugary drinks, no processed snacks. Exercise: 150 minutes a week, supervised if possible. GLP-1 drugs start low - 0.25 mg a week - and slowly increase over 16 to 20 weeks to minimize side effects.
Nausea? Many clinics now give patients vitamin B6 (pyridoxine) at 25 mg twice a day. It helps in about two-thirds of cases. Meal replacement shakes? They boost adherence to 78% compared to standard advice. And while rare, doctors watch for signs of pancreatitis - about 3 in 1,000 patients per year.
What’s Next?
The market for MASLD treatments is exploding - worth nearly $15 billion in 2023 and projected to double by 2030. Semaglutide leads the pack, but new drugs like tirzepatide (Mounjaro) are showing even better weight loss results. The FDA just approved resmetirom for MASH, expected to launch in early 2024. This drug targets liver scarring directly. Soon, doctors may combine it with GLP-1 drugs for patients with advanced disease.But here’s the hard truth: we’re still behind. Only 28% of rural U.S. counties have a specialist who knows how to treat MASLD. Most people still get diagnosed by accident - during a routine blood test or ultrasound for something else. And while GLP-1 drugs work wonders, they’re expensive - over $1,200 a month. Insurance coverage is patchy. Medicare covers about two-thirds of patients for obesity, but many private plans still treat it as cosmetic.
By 2030, MASLD could become the top reason for liver transplants in the U.S. - even more than hepatitis C. That’s not inevitable. It’s preventable. But only if we treat it early, seriously, and with the right tools.
What You Can Do Today
If you’ve been told you have fatty liver:- Don’t panic. But don’t ignore it either.
- Get a FibroScan or liver fat scan if you can. Know your baseline.
- Start losing weight - even 5% helps. Aim for 10%.
- Move more. Walk 30 minutes a day, five days a week.
- Cut out sugary drinks. That includes fruit juice. Fructose is a major driver.
- If you have type 2 diabetes or obesity, talk to your doctor about GLP-1 agonists. They’re not a magic bullet, but they’re the most effective drug option we have right now.
- Ask for support. Dietitians, support groups, structured programs - they make all the difference.
This isn’t about being thin. It’s about being healthy. Your liver doesn’t care about your size. It cares about what you eat, how much you move, and whether you treat the root cause - not just the symptom.
Can you reverse fatty liver without losing weight?
No - not reliably. While some people see minor improvements with diet changes or supplements, studies show that only sustained weight loss of at least 5% leads to measurable fat reduction in the liver. For inflammation and scarring, 10% or more is required. There are no proven alternatives that match the effectiveness of weight loss.
Are GLP-1 drugs safe for the liver?
Yes - and they’re actually helping the liver. GLP-1 receptor agonists like semaglutide and liraglutide reduce liver fat, inflammation, and scarring in people with MASLD. Rare cases of liver enzyme spikes have been reported, but these are usually mild and reversible. The drugs are not linked to liver damage. In fact, they’re one of the few treatments proven to improve liver health.
How long do you need to take GLP-1 drugs for fatty liver?
There’s no fixed timeline. Most people need to stay on the medication long-term to maintain weight loss and liver benefits. Stopping often leads to weight regain and return of liver fat. Some patients who lose 10%+ and keep it off with lifestyle changes may be able to taper off under medical supervision - but this is still being studied. For now, think of GLP-1 drugs as a tool to help you reach a healthier state - not a cure you take for a few months.
Is MASLD the same as alcoholic liver disease?
No. MASLD is caused by metabolic problems like obesity and insulin resistance - not alcohol. Even people who drink very little or not at all can develop it. The key difference is the cause. Alcoholic liver disease requires a history of heavy drinking. MASLD doesn’t. That’s why the name changed - to reflect the real source of the problem.
Can you take GLP-1 drugs if you don’t have diabetes?
Yes. Semaglutide (Wegovy) and liraglutide (Saxenda) are FDA-approved specifically for chronic weight management in people without diabetes. They’re prescribed based on BMI and metabolic risk - not blood sugar levels. If you have MASLD and obesity, you’re a candidate, regardless of whether you have type 2 diabetes.
What’s the best diet for MASLD?
The Mediterranean diet is the most studied and recommended. Focus on vegetables, whole grains, lean protein, olive oil, nuts, and fish. Avoid added sugars, especially fructose from soda and sweetened foods. Limit processed carbs. Reduce saturated fats. Studies show this diet reduces liver fat better than low-fat diets. You don’t need to count calories rigidly - just eat real food, stop eating when you’re full, and cut out the junk.

8 Responses
Losing 10% of your body weight can literally reverse liver damage. That’s not hype-that’s science. I’ve seen it in my own family. My dad dropped 18 pounds over a year, stopped drinking soda, and his FibroScan numbers improved so much his doctor was stunned.
Been on semaglutide for 8 months. Lost 14%. Nausea was brutal at first but B6 helped. Still take it. Liver fat down 60%. No regrets. Just wish it wasn’t so damn expensive.
The real issue isn’t the drug or the diet-it’s the systemic neglect of metabolic health in modern medicine. We treat symptoms, not root causes. MASLD is a mirror of our food system, our sedentary culture, and our refusal to see obesity as a disease. GLP-1s are a bandage on a hemorrhage. We need policy change, not just prescriptions.
And yet… here we are. I’m grateful for the drugs. But I’m furious we got here in the first place.
While the science is compelling, it’s important to acknowledge that not everyone has access to specialists, FibroScans, or $1,200/month medications. For many, the most realistic step is cutting out sugary drinks and walking 30 minutes a day. Small changes matter. Progress, not perfection.
Also, vitamin B6 for nausea? That’s a gem. I’ll be sharing that with my patients tomorrow.
Just got diagnosed with MASLD last month. I’m 42, overweight, and terrified. But reading this? I feel seen. Not judged. I’m starting the Mediterranean diet this week. No more juice. No more snacks. Just real food. I’m not doing this to look good-I’m doing it to not die before my kids graduate high school.
Let’s be real-GLP-1s are just the latest pharmacological fad for the lazy elite. 🤡 You want to fix your liver? Stop eating processed garbage and move your ass. No drug replaces discipline. Also, ‘MASH’? So trendy. Next they’ll call it ‘Metabolic Dysfunction-Associated Overindulgence Syndrome’ 😏
My cousin lost 20% on Ozempic, then stopped. Gained it all back in 6 months. Now his liver’s worse than before. He thinks the drug was the cure. It wasn’t. It was a tool. He didn’t change his relationship with food. He just outsourced the willpower. And now he’s paying the price. 🙃
People need to understand: this isn’t a quick fix. It’s a lifelong recalibration. If you’re not ready for that, don’t start.
Just wanted to say thank you for writing this. I’ve been struggling for years. I thought I was alone. Seeing someone actually explain what’s happening to my liver-it helped me stop feeling ashamed. I’m starting with cutting out soda tomorrow. One step at a time.