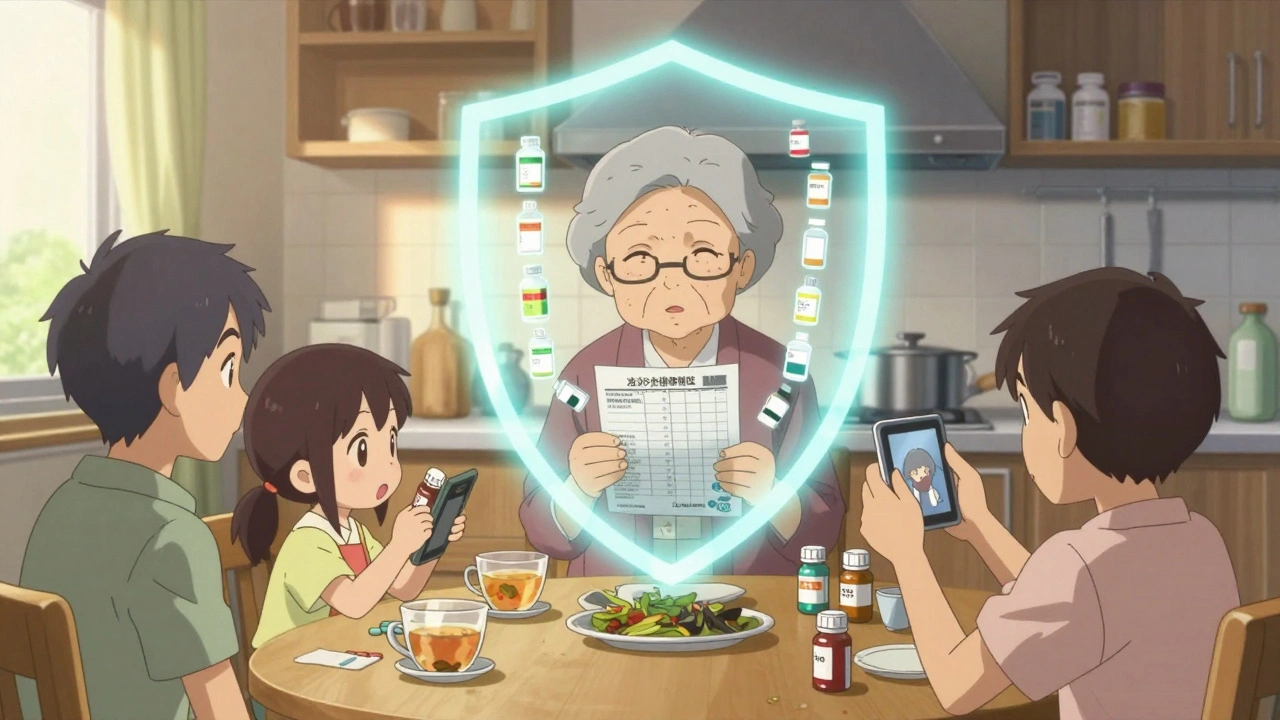
Every year, tens of thousands of people in the U.S. end up in the hospital or worse because of a simple mistake: someone didn’t know what medications they were taking. It’s not about forgetting a pill. It’s about not telling your doctor about the turmeric supplement you take for joint pain, or the ibuprofen you pop for headaches, or the herbal tea your aunt swears by for sleep. These aren’t just "natural" extras. They can turn a safe prescription into a dangerous mix. The good news? You can stop this before it happens-with one clear, updated list and the habit of sharing it.
Why Your Medication List Matters More Than You Think
If you’re taking five or more medications, you’re not alone. Nearly 40% of adults over 65 are. But here’s the problem: the more pills you take, the higher your risk of a dangerous interaction. A drug you’ve been on for years might suddenly react badly with something new-like a blood thinner and St. John’s Wort, which can cause dangerous bleeding. Or a common painkiller like ibuprofen making your blood pressure meds less effective. These aren’t rare accidents. They’re preventable.The data is clear: when patients share a full, accurate list of everything they take, adverse drug events drop by 35% to 50%. That’s not a small win. That’s life-saving. And it’s not just about prescriptions. Over-the-counter meds, vitamins, supplements, and even herbal teas are responsible for 30% of serious drug interactions. Yet most people forget to mention them-until it’s too late.
What Goes on a Complete Medication List
A good list isn’t just a scribble on a napkin. It needs details. Here’s what to include for every item:- Exact name: Both brand and generic. Example: "Lisinopril 10 mg" (brand: Zestril)
- Dosage: How much? 5 mg? 500 mg? Don’t say "one pill"-say "10 mg tablet"
- Frequency: Once daily? Twice a day? Every 8 hours?
- Route: Oral? Patch? Injection? Inhaler?
- Why you take it: "For high blood pressure," "for anxiety," "for arthritis pain"
- Start date: When did you begin taking it?
- Prescribing provider: Doctor’s name and clinic
- Special instructions: "Take on empty stomach," "avoid grapefruit," "take with food"
And don’t forget the non-prescription stuff:
- Over-the-counter drugs: "Tylenol Extra Strength 500 mg," "Nexium 20 mg," "Robitussin DM"
- Vitamins and minerals: "Vitamin D3 2000 IU," "Magnesium glycinate 400 mg"
- Herbal supplements: "St. John’s Wort 300 mg," "Ginger root 500 mg," "Turmeric 500 mg"
- Allergies: "Penicillin-causes hives and swelling," "Sulfa drugs-rash and fever"
Even if you think it’s "not medicine," if it’s something you swallow, inject, or inhale regularly, it belongs on the list.
How to Keep Your List Updated
A list that’s outdated is worse than no list at all. It gives false confidence. Here’s how to keep it current:- Update within 24 hours of any change-new prescription, stopped med, changed dose
- Review the whole list once a month. Ask yourself: "Did I start anything new? Did I stop anything?"
- Take a photo of every pill bottle. Store them in a folder on your phone. It’s faster than typing and harder to forget.
- Use free tools like the FDA’s "My Medicine Record" form or apps like Medisafe or MyMeds. They send reminders and let you share digitally.
Don’t rely on memory. Don’t rely on your pharmacy’s system. They don’t always know what you’re taking over the counter. Only you know your full picture.

How to Share It-And When
Having the list is only half the battle. You have to give it to the right people at the right time.- Bring it to every appointment-even if you’ve been there before. Don’t wait for them to ask. 63% of providers don’t routinely request a full list.
- Hand it to the nurse or receptionist when you check in. Say: "Here’s my updated medication list. Could you make sure my doctor sees it?"
- If you’re seeing multiple specialists, pick one primary provider to be your "medication coordinator." They can help spot overlaps or conflicts.
- At the ER or urgent care, show the list. Don’t just say "I take a bunch of stuff." Show them the paper or phone screen.
- If you’re hospitalized, give a copy to every nurse who comes in. Ask: "Can you check this against what’s in your system?"
Some people worry about being "annoying." But if you’re taking multiple meds, you’re not being annoying-you’re being smart. Providers who ignore your list are the ones taking risks.
What Doesn’t Work (And Why)
Not all methods are equal. Here’s what’s flawed:- Just trusting your pharmacy’s list: Pharmacies track prescriptions well-but only 45% of OTC meds and supplements show up in their records.
- Only using your EHR portal: Your doctor’s electronic system might miss what you buy at the grocery store.
- Writing it on a sticky note: It gets lost, smudged, or forgotten. A paper list kept in your wallet has only 62% accuracy in emergencies.
- Assuming your doctor "knows" your meds: A 2022 study found 43% of medication errors happen during care transitions-when you switch doctors or go to the hospital.
The most effective approach? A combo: digital backup (phone app or PDF), printed copy in your wallet, and a photo of each bottle on your phone. That way, you’re covered no matter what.
What to Ask Your Provider
Don’t just hand over the list and walk away. Use it to start a conversation. Ask:- "Could any of these medications interact with each other?"
- "Are there any foods, drinks, or supplements I should avoid?"
- "Is there anything here I might not need anymore?"
- "Could this be causing my fatigue/dizziness/upset stomach?"
Pharmacists are your secret weapon. They’re trained to spot interactions. If you get your prescriptions filled at an independent pharmacy, ask for a free medication review. A 2023 study found pharmacist-led reviews reduced inappropriate prescribing by 32% in older adults.
Real Stories, Real Results
One woman in Ohio brought her list to her cardiologist. She’d been taking warfarin for a blood clot and daily St. John’s Wort for depression. Her doctors never asked about the supplement. The pharmacist spotted it immediately-St. John’s Wort reduces warfarin’s effect by up to 60%. Without intervention, she could’ve developed a clot. That list saved her life.Another man in Florida had been taking metformin for diabetes and ibuprofen for back pain. He didn’t think the painkiller mattered. But ibuprofen can damage kidneys, especially when combined with metformin. His pharmacist flagged it and suggested acetaminophen instead. His kidney function stabilized.
These aren’t rare cases. They’re the norm. And they’re preventable.
What’s Changing in 2025
The system is catching up. New federal rules now require patient portals to show your full medication list-including what you report yourself. The FDA has updated labels on 120 drugs to include clearer warnings about food and supplement interactions. AI tools like IBM Watson Health are now detecting interactions with 94% accuracy in clinical tests.But none of this matters if you don’t keep your list updated and share it. Technology helps-but only if you’re the one driving it.
The bottom line: Your medication list isn’t paperwork. It’s your safety net. The more you take, the more vital it becomes. Don’t wait for an emergency to realize you didn’t tell someone what you were really taking. Update it. Print it. Show it. Ask the questions. You’re not just managing pills-you’re managing your health.
What if I forget to bring my medication list to my appointment?
If you forget, ask for a paper form at the front desk or use your phone to pull up your digital list. Most clinics have templates you can fill out on-site. But don’t rely on memory-write down what you take as soon as you can, even if it’s just a note on your phone. The next time you go, bring it. Over time, it becomes routine.
Do I need to list vitamins and supplements even if they’re "natural"?
Yes. "Natural" doesn’t mean safe. St. John’s Wort can interfere with blood thinners, antidepressants, and birth control. High-dose vitamin K can undo the effect of warfarin. Turmeric and ginger can increase bleeding risk when taken with aspirin or NSAIDs. These aren’t harmless. They’re active substances that interact with your body-and your prescriptions.
Can my pharmacy help me keep track of everything?
Yes, but only for prescriptions. Pharmacies can flag interactions between your written prescriptions. But they won’t know about the melatonin you take at night or the omega-3s you bought online unless you tell them. Always share your full list with your pharmacist during your refill visits. Many offer free medication reviews-take advantage.
How often should I update my medication list?
Update it within 24 hours of any change-new med, stopped med, changed dose. Do a full review once a month. Set a reminder on your phone for the first of every month. During that review, check expiration dates, refill status, and whether you still need each item. If you’re unsure, ask your pharmacist or doctor.
Is it safe to share my medication list digitally?
Yes, if you use secure apps like Medisafe, MyMeds, or your health system’s patient portal. Avoid sending PDFs via text or unsecured email. Use password-protected apps with encryption. If you’re using a photo of your pill bottles, store them in a locked folder on your phone or cloud account. Your health data is private-and you have the right to protect it.
What if my doctor doesn’t seem to care about my list?
Politely insist. Say: "I’ve had bad reactions before, so I make sure every provider sees this list. Can you please review it with me?" If they dismiss it repeatedly, consider finding a new provider. A good doctor will welcome your involvement. Your safety isn’t optional.


12 Responses
Been using Medisafe for a year now. Set it up after my grandma almost got hospitalized from mixing warfarin and ginkgo. Best thing I ever did. Now I get alerts when something’s about to expire or when I miss a dose. Even my pharmacist says it’s the cleanest list he’s seen.
Don’t wait for a crisis. Just do it.
It takes five minutes.
And it might save your life.
I’m a nurse in a rural clinic. I’ve seen this too many times. Old folks come in with five pill bottles, a bag of supplements, and zero idea what’s in them. One lady brought a jar labeled ‘Grandma’s Sleep Blend’ - turned out to be valerian, kava, and melatonin in equal parts. Her BP was in the toilet.
Don’t underestimate the ‘natural’ stuff. They’re drugs too. Just without the FDA sticker.
My mom writes everything on a sticky note and sticks it to the fridge. Lost it twice. Now she uses the Notes app on her iPhone. Takes two minutes. She even added her allergies. Simple. No drama. Just works.
Of course the government wants you to track your pills. Next they’ll make you log your breathing and bowel movements. This isn’t medicine. It’s surveillance dressed up as safety. You think your doctor actually reads this stuff? Nah. They’re too busy scrolling TikTok between patients. You’re just feeding the machine.
Let’s not forget the philosophical underpinnings of pharmaceutical autonomy - the individual’s moral imperative to maintain ontological integrity in the face of institutionalized medical hegemony. The modern pharmacological landscape is a labyrinth of commodified bio-power, where the body becomes a site of administrative control, and the medication list - that brittle, paper-thin artifact - is the last vestige of self-sovereignty. In an age where algorithms decide your insulin dosage, and AI predicts your depression before you feel it, the act of writing down your supplements becomes a quiet, radical act of resistance. You are not a data point. You are the curator of your own physiology. And if you don’t document it? Then you’ve already surrendered.
I love how this post doesn’t just tell you what to do - it shows you why it matters. I used to think my vitamins were harmless. Then I started reading about how turmeric affects blood clotting. Now I show my list to every provider, even the acupuncturist. It’s not about being annoying. It’s about being responsible. And honestly? It’s kind of empowering to know you’re the only one who really knows what’s in your body.
Did you know the FDA doesn’t even test herbal supplements before they hit the shelves? They just assume they’re safe until someone dies. And your doctor? They’re paid by Big Pharma to ignore the ‘natural’ stuff. That’s why they don’t ask. That’s why your pharmacy doesn’t track it. It’s all a cover-up. The real danger isn’t the interaction - it’s the silence. They want you dependent on pills they control. Your list? That’s your weapon. Print it. Laminate it. Carry it like a shield.
It’s irresponsible to suggest that patients should be responsible for managing their own medication lists. That’s the job of the medical professional. If your doctor doesn’t know what you’re taking, that’s a failure of the system - not a failure of your memory. We’ve outsourced accountability to the patient because the healthcare system is broken. But don’t let them make you feel guilty for it. You’re not the problem. The bureaucracy is.
OMG YES. I just got off the phone with my pharmacist and she said I was taking TWO different things for acid reflux. I didn’t even realize. I’m so glad I printed my list. I’m gonna start doing it every month. And I’m telling all my friends. This is life or death. Seriously. I almost missed it. Don’t be like me. Do it now.
The cognitive load of managing polypharmacy is often underestimated. The meta-cognitive awareness required to maintain an accurate, dynamic pharmacological inventory - especially in the context of fragmented care delivery systems - imposes a significant burden on individuals who are already navigating chronic conditions. When we privilege the patient as the primary custodian of this data, we are implicitly assuming a level of health literacy, temporal capacity, and digital access that is not universally distributed. The solution isn’t merely individual action - it’s systemic integration. We need interoperable, patient-centered EHRs that auto-populate from pharmacy records, OTC databases, and wearable biometrics. Until then, yes - keep the list. But don’t mistake personal diligence for systemic justice.
My cousin took a supplement called ‘Immune Boost’ and ended up in the ER. Turns out it had hidden steroids. No label. No warning. Just a bottle from some guy on Instagram. So yeah - write your list. But also stop buying crap from the internet. That’s the real problem. Not the list. The gullibility.
Why do you think they want you to track everything? So they can charge you more. Every time you mention a supplement, they slap on a ‘high-risk’ tag and raise your premiums. This isn’t safety. It’s profit. And the more you comply, the more they own you. Just stop taking everything. Let your body heal itself. That’s what nature intended.