Why Your Medication Review Appointment Matters
It’s not just another doctor’s visit. A medication review is a safety check for everything you’re taking - pills, inhalers, creams, vitamins, even herbal teas. If you’re on five or more medications, or if you’ve seen multiple doctors recently, this appointment could prevent a serious reaction, hospital stay, or even save your life. In the UK, practices like Godiva Group Practice NHS now treat these reviews as mandatory, not optional. If you skip them, your repeat prescriptions could be stopped until you attend.
These reviews aren’t about blaming you for forgetting a dose. They’re about making sure your medicines actually work together - and don’t hurt you. Pharmacists and GPs now lead most of these appointments, especially for older adults or people with long-term conditions like diabetes, heart disease, or Parkinson’s. The goal? To cut out what’s unnecessary, fix what’s risky, and keep what’s helping.
What to Bring: Your Medicine Bag
Don’t just list your medicines. Bring them. All of them.
- Every prescription bottle - even if you haven’t opened it yet
- Over-the-counter painkillers like ibuprofen or paracetamol
- Vitamins, supplements, and herbal remedies (even if you think they’re harmless)
- Inhalers, eye drops, creams, patches, and liquid medicines
- Any medicines you’ve stopped taking recently
The Northern Health and Social Services Board in Ireland says: “By medicines we mean anything you take.” That includes the ginger tea you drink for digestion or the magnesium tablets your friend swore by. If you didn’t get it from a pharmacy, it still counts. Why? Because these can interact with your prescriptions. St John’s Wort, for example, can make blood thinners or antidepressants stop working.
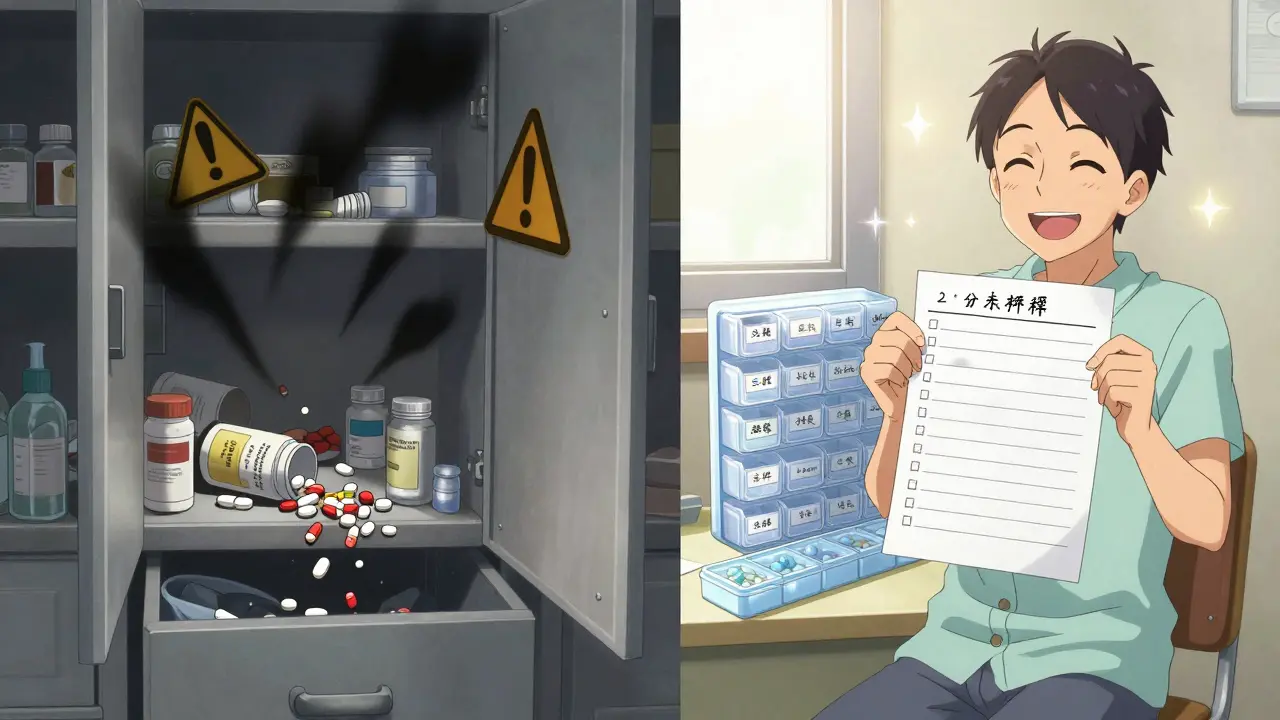
Don’t rely on memory. A 2023 study showed that patients forget or misremember up to 40% of their medications when asked verbally. Bring the real bottles. The pharmacist will check expiry dates, dosages, and whether you’re still using them.
Make a Written List - Even If You Bring the Bottles
Write down each medicine with four details:
- Name: Full name - not “the blue pill.” Write “Metformin 500mg” or “Salbutamol inhaler (100mcg/dose)”
- Dose: How much you take - “Take one tablet twice a day after breakfast and dinner”
- Why you take it: “For high blood pressure,” “For joint pain,” “For sleep”
- Who prescribed it: “Dr. Patel, GP,” “Cardiologist at Heartland Clinic”
Include side effects you’ve noticed. Did you get dizzy after starting a new blood pressure drug? Did your stomach ache after the antibiotic? Did your muscles feel stiff after a statin? Write it down. These aren’t complaints - they’re clues. Your GP might spot a pattern you didn’t even connect.
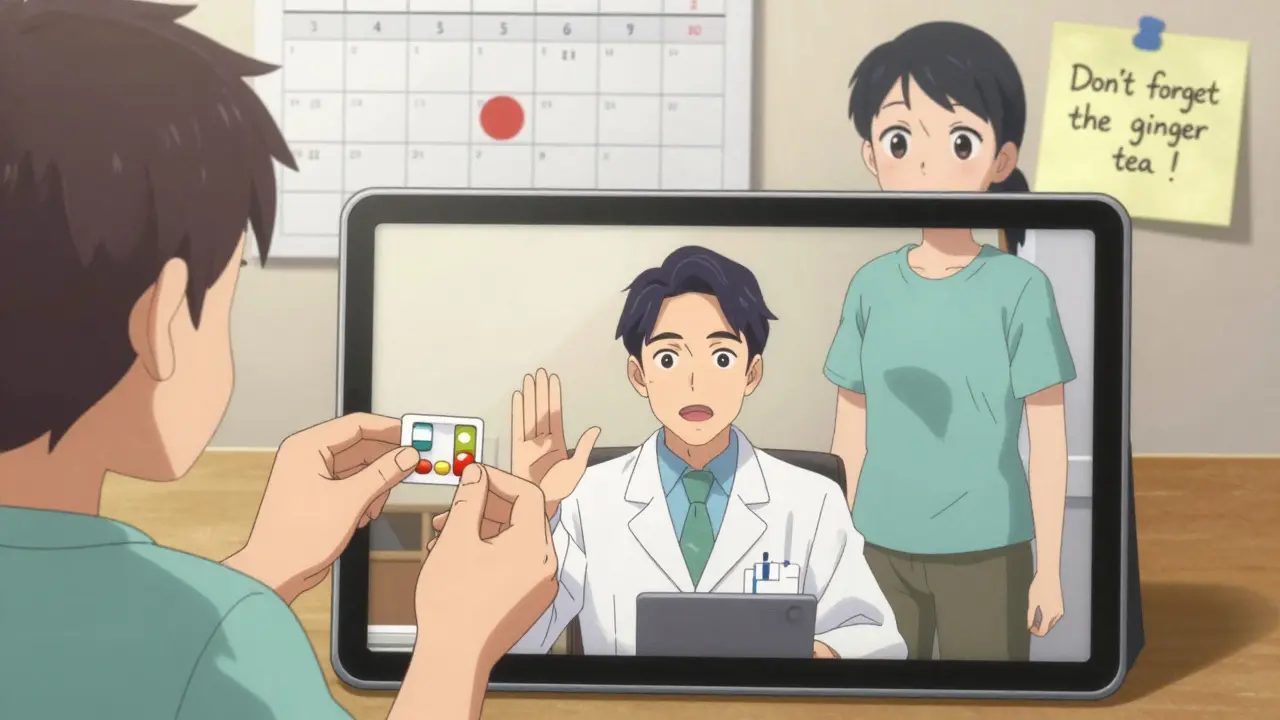
For people with Parkinson’s, timing matters more than ever. Medications like Levodopa need to be taken within 30 minutes of each other. If you’re doing a video call, your pharmacist won’t see your pill organizer. Your list becomes your lifeline.
Think About Your Goals - What Do You Want to Change?
A medication review isn’t just the doctor asking questions. It’s a conversation. You get to ask too.
Before your appointment, think about:
- Are you taking too many pills each day? Could any be cut out?
- Do you struggle to remember when to take them?
- Have you had side effects that make you want to stop?
- Are you paying too much for medicines you don’t think are working?
- Do you feel like your condition isn’t improving?
Write down two or three things you want to talk about. Example: “I’ve been taking amitriptyline for nerve pain for five years, but I’m always sleepy. Can we try something else?” or “I’m on eight different pills. Is there any way to reduce that?”
The Health Innovation Network calls this “shared decision-making.” Your input isn’t optional - it’s essential. If you don’t speak up, they might assume everything’s fine.
What If You Can’t Get to the Clinic?
Telehealth reviews are now common. But they need more prep.
If you’re doing a video or phone call:
- Have all your medicines ready on the table in front of you
- Test your camera and mic before the call - don’t wait until the minute before
- Have your list printed out or open on a second screen
- Ask someone to sit with you if you’re worried about remembering everything
Patients with memory issues or mobility problems can request home visits. The Northern Health and Social Services Board says you need to ask for this when booking - it won’t be offered automatically. Don’t assume you’re too busy or too unwell. Say it: “I need a home visit because I can’t travel.”
What Happens During the Appointment?
It’s not a lecture. It’s a problem-solving session.
Your clinician will:
- Check your list against your prescription records
- Look for overlaps - two drugs doing the same thing
- Spot interactions - like warfarin and garlic supplements
- Ask if you’re taking medicines as directed
- Discuss whether any drugs are no longer needed
- Explain side effects you might not have connected to your meds
- Offer alternatives - cheaper options, easier forms (like patches instead of pills)
They might suggest stopping one drug, lowering a dose, or switching to a different one. You don’t have to agree right away. Ask: “What happens if I don’t change anything?” or “What’s the risk of stopping this?”
At the end, you should walk out with a clear plan: what stays, what goes, what changes, and when. Get it in writing.
What If You’re Asked to Stop a Medicine?
It’s normal. Sometimes, a drug prescribed years ago is no longer needed. Or it’s causing more harm than good.
But don’t stop anything on your own. Even if your doctor says “you can stop,” they’ll usually give you a plan:
- Gradual tapering - slowly reducing the dose over weeks
- Monitoring - checking your blood pressure, mood, or symptoms after stopping
- Follow-up - booking another appointment in 4-6 weeks to see how you’re doing
Some medicines, like antidepressants or steroids, can cause serious withdrawal if stopped suddenly. Your doctor knows this. But you need to trust the process.
What Happens If You Don’t Go?
It’s not just about missing a check-up. There are real consequences.
Godiva Group Practice NHS has a clear policy: after sending three monthly reminders, they limit your repeat prescriptions to a one-month supply. If you still don’t attend, they stop prescribing altogether - until you complete the review.
Why? Because polypharmacy is dangerous. The more medicines you take, the higher your risk of falls, confusion, kidney damage, or dangerous interactions. A 2021 review found that 1 in 5 hospital admissions in people over 65 were caused by medication problems - many of which could’ve been caught in a simple review.
This isn’t punishment. It’s protection. Your practice isn’t trying to control you. They’re trying to keep you safe.
After the Appointment: What to Do Next
Don’t just leave with a smile and a new prescription. Do this:
- Ask for a printed copy of your updated medication list
- Confirm who to contact if side effects get worse
- Write down the next review date - usually once a year
- Update your list if you start or stop anything, even a new painkiller from the chemist
- Share your updated list with any other doctors or specialists you see
Keep your list in your wallet, phone notes, or with your medical records. If you ever go to A&E or see a new doctor, show them this list. It could prevent a life-threatening mistake.
Final Tip: Make It Routine
Think of your medication review like an annual MOT for your body. You don’t wait until your car breaks down to check the oil. Don’t wait until you feel awful to check your medicines.
Set a calendar reminder for your next review. If you’re on multiple meds, it’s not a luxury - it’s part of your health care. And if you’re unsure about anything - even after the appointment - call your practice. No question is too small. Your safety is worth it.


14 Responses
This is such an important guide! I work as a geriatric pharmacist, and I can't tell you how many times I've seen patients come in with 12+ meds they're not even sure why they're taking. Bringing the actual bottles? Game-changer. So many times, the bottle says 'take at bedtime' but the patient's been taking it at breakfast for years. Also, don't forget to mention that some OTCs like antihistamines can make dementia worse. This post should be required reading for every senior.
Simple advice works best. Bring your pills. Write down why you take each one. Talk to your doctor. Don't be shy. Your life matters. Many people forget this. You don't need to be smart. Just be honest. Your body tells you when something is wrong. Listen.
Oh please. 'Mandatory' reviews? That's just another way for Big Pharma and the NHS to control you. You think they care about your safety? They care about liability. I know a guy whose blood thinner was stopped because he took turmeric. Turmeric! And now he's having clots. This is medical tyranny. They don't want you to be healthy-they want you dependent on their system. Wake up.
Okay so I had my med review last month and honestly? It was kind of a vibe. I brought like 17 bottles and my grandma's herbal tea that she swears fixes her arthritis (it's chamomile and ginger, btw) and the pharmacist just laughed and said 'this is why I love my job.' We ended up cutting three things I hadn't taken in two years, switched one for a patch because I keep forgetting pills, and I got a free pill organizer. I didn't even know I was supposed to ask about cost-I just assumed I had to pay for everything. Also, my doc said my 'sleep aid' was probably making my anxiety worse. Who knew? I'm now drinking warm milk and listening to whale sounds. It's weird but it works. Also, I cried. Not because I was sad. Because I felt seen. Like, really seen. And I didn't even know I needed that.
I'm so glad this exists. My mom is 78 and on 9 meds. She used to get confused and take double doses. After this review, they switched her to a blister pack and set up weekly calls. She says she feels 'lighter.' I didn't realize how much stress it was for her. You don't have to be a genius to do this. Just show up. And if you're scared? Bring someone. You're not alone. 💙
I LOVE this! 🙌 Seriously, this should be on every pharmacy wall. I'm a nurse and I've seen so many people get hospitalized because they didn't know that St. John's Wort and antidepressants don't play nice. And the part about bringing the bottles? YES. I had a patient once who said 'I take the white pill' and it turned out she was taking a sugar pill because her real one expired and she was too embarrassed to say. We fixed it. She cried. We hugged. It was beautiful. 🤗❤️
I just had my review last week. I was nervous. But the pharmacist was so chill. We talked like two humans, not like a doctor and a patient. She asked me if I felt like I was taking too many pills. I said yes. She didn't judge. She just said 'let's see what we can do.' We cut two things I didn't need anymore. One was a vitamin I'd been taking since 2018. I didn't even remember why I started it. It felt like a weight lifted. Thanks for the reminder to be honest.
They're lying. They're not protecting you. They're protecting their insurance premiums. They don't want you healthy. They want you on lifelong meds. That's why they make it mandatory. They profit from dependency. Don't be fooled. Your pills are poison. Your body knows. Stop listening.
This is a textbook example of paternalistic medical overreach. The notion that patients are incapable of managing their own regimens is not only condescending-it is dangerous. The idea that 'herbal teas' are equivalent to pharmaceuticals in risk profile is scientifically absurd. Many of these 'interactions' are statistically negligible. The real issue is systemic underfunding of primary care, which forces practitioners to outsource responsibility to patients. This is not safety. It is administrative burden repackaged as public health.
One must question the epistemological foundations of this 'guide.' The assumption that physical containers-bottles, vials, blister packs-constitute ontological truth regarding pharmacological adherence is a fallacy rooted in Cartesian materialism. One cannot reduce the phenomenology of self-medication to the mere aggregation of pharmaceutical artifacts. Furthermore, the invocation of 'Northern Health and Social Services Board' as an authoritative source is a rhetorical sleight-of-hand, masking the neoliberal restructuring of healthcare into performative compliance. The real issue? The commodification of wellness.
I brought my meds. I wrote the list. I didn’t say anything. They didn’t ask. I left with the same pills. I didn’t feel heard. I think I’m not the only one. Maybe we need better training for the people doing these reviews. Not just checklists.
I am appalled by the casual dismissal of pharmacological science in this article. The suggestion that 'ginger tea' is on par with warfarin in terms of clinical risk is not only misleading-it is grossly irresponsible. The pharmacokinetics of herbal supplements are not regulated, but that does not mean they are benign. Moreover, the emphasis on 'bringing bottles' as a primary intervention ignores the role of electronic health records, medication reconciliation software, and pharmacist-led medication therapy management-tools that have demonstrably reduced adverse drug events by 47% in peer-reviewed studies. This piece is not a guide-it is a disservice to evidence-based practice.
i brought my meds but forgot to write down why i take them. i just said 'for my heart' and they asked me to be more specific. i felt dumb. i didn't know the names. now i know. it's metoprolol. i didn't know that. also, i think i was supposed to bring my blood pressure log but i didn't. i'm going next month. i'll do better. sorry for the typos.
In the grand tapestry of human health, this review process is but a single thread. Yet, it reveals a deeper truth: we have lost the art of listening-to our bodies, to our medicines, to each other. The bottle is not the medicine. The intention behind its use is. Are we treating symptoms? Or are we healing the whole? The real revolution is not in the checklist, but in the quiet courage to say: 'I am not sure this is working for me.' That is the first step toward true autonomy.