When someone you care for takes five or more medications a day, keeping track isn’t just helpful-it’s life-saving. Over 40% of older adults in the U.S. are managing polypharmacy, and each extra pill increases the risk of dangerous side effects, missed doses, or deadly interactions. A well-organized medication list cuts through the confusion. It’s not about being perfect. It’s about being ready.
What Goes on a Medication List
A good medication list isn’t just a note scribbled on a napkin. It’s a detailed, accurate record that every doctor, pharmacist, and caregiver can trust. Start with the basics for every single item-prescription, over-the-counter, or supplement.- Medication name: Write both the brand name (like Lipitor) and the generic (atorvastatin). Pharmacists use the generic to avoid mix-ups.
- Dosage: Be exact. Not “one pill,” but “Lisinopril 10mg.”
- Frequency: “Twice daily,” “every 8 hours,” or “as needed for pain.” Don’t assume everyone knows what “QID” means.
- Purpose: Why are they taking it? “For high blood pressure,” “for arthritis pain,” “for sleep.” This helps spot duplicates or unnecessary drugs.
- Special instructions: “Take with food,” “do not crush,” “avoid grapefruit,” “take on empty stomach.” These details prevent side effects.
- Start date: When did they begin this medication? This helps track changes over time.
- Prescribing doctor: Who wrote the script? Name and phone number.
- Pharmacy contact: Name, address, and phone of the pharmacy filling the prescription.
- Side effects to watch for: Write down the top 2-3 risks. For example, “dizziness,” “stomach bleeding,” “confusion.”
- Allergies: List every known reaction-rash, swelling, trouble breathing. Include the medication that caused it.
- Stop date: For time-limited prescriptions like antibiotics or short-term pain meds, note when they should end. Many seniors keep taking these long after they’re needed.
Don’t forget the National Drug Code (NDC) number-it’s on the bottle and helps pharmacists match exact pills. If you can’t find it, call the pharmacy. It’s worth the five-minute call.
Choose Your Format: Paper, Digital, or Both
There’s no one-size-fits-all solution. The best format is the one you’ll actually use and update.Paper lists still work for 63% of caregivers. They’re simple, don’t need batteries, and can be handed to an ER doctor in seconds. Use a three-ring binder with tabs for medications, appointments, and questions. Laminate the main list so it won’t smudge or tear. Many caregivers swear by the “brown bag method”-bring every pill bottle to each appointment. It’s messy, but it works.
Digital tools like Medisafe, MyMeds, or even a shared Google Sheet are better for complex regimens. If someone takes more than four medications, digital systems reduce errors by 42%. They can send reminders, track refills, and sync with pharmacies. CVS and Walgreens now offer free sync services that auto-update your list when prescriptions are filled.
But here’s the catch: 62% of caregivers over 65 find apps too hard to use. And 71% quit digital tools within three months because they’re too time-consuming. So don’t go digital unless you’re comfortable with it. If you are, use a tablet or phone with a large screen. Turn on voice-to-text so you don’t have to type everything.
The smartest approach? Use both. Keep a laminated paper copy in a visible spot-like on the fridge or next to the medicine cabinet. Keep a digital backup on your phone, synced with a trusted family member. That way, if the power goes out or the phone dies, you still have the list.
Step-by-Step: How to Build Your List
Building a complete list takes time. Don’t rush it. Follow these six steps.- Collect everything: Go through every drawer, cabinet, and bedside table. Gather every pill bottle, cream tube, inhaler, and supplement jar. Include vitamins, herbal teas, and CBD oils. You’d be surprised what’s hiding.
- Write down each item: Use the 12-point checklist above. Don’t guess. If you’re unsure what something is, call the pharmacy. Take a photo of the label if needed.
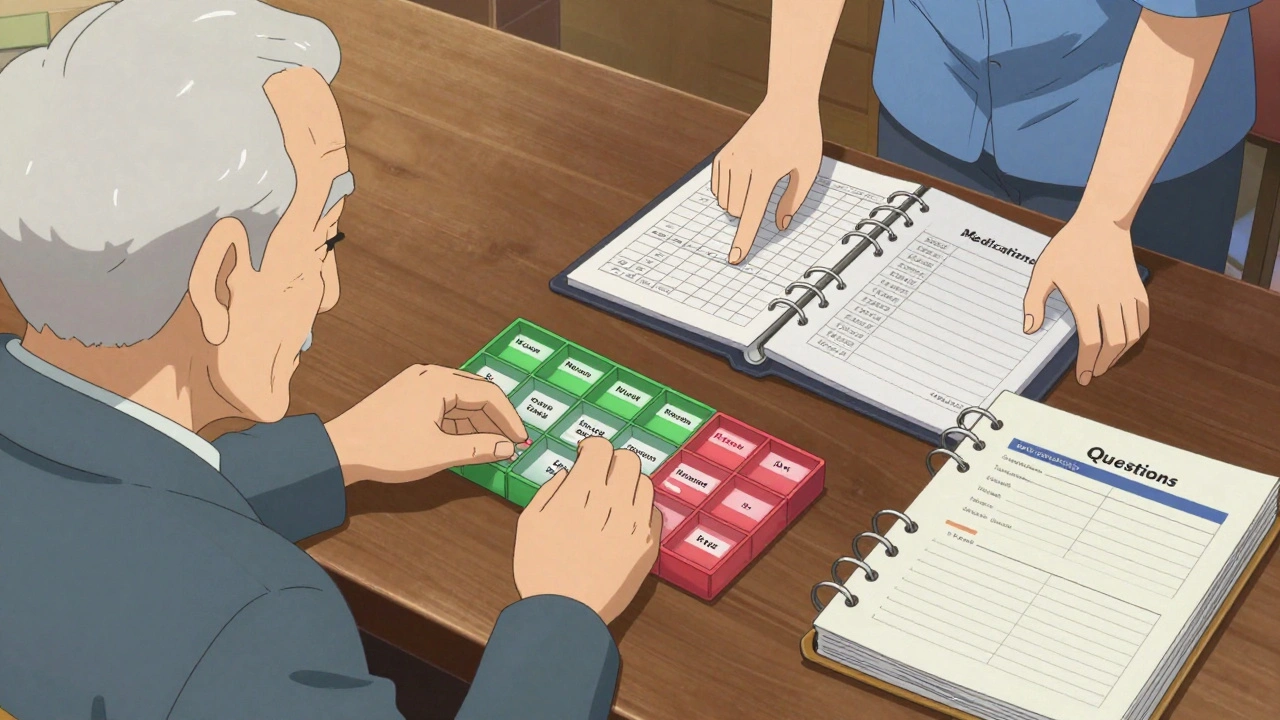
- Sort by time of day: Group medications by when they’re taken-morning, noon, evening, bedtime. This helps avoid confusion. Use color-coded stickers: blue for morning, red for night.
- Create two copies: One printed for home, one saved digitally. Email the digital copy to all caregivers and the primary doctor.
- Set a weekly update rule: Every Sunday evening, spend 15 minutes reviewing the list. Did anything change? Did the doctor add, remove, or change a dose? Update it immediately. Don’t wait.
- Share with everyone: Give a copy to every provider-even the dentist. If your loved one sees five different specialists, make sure they all have the same list. Designate one person as the “medication coordinator” to avoid conflicting advice.
The first month is the hardest. Caregivers make an average of 4.7 errors in the first 30 days. That’s normal. You’re learning. After that, it becomes routine.
Handling the Hard Parts
Some medications are trickier than others.“As needed” meds: These are the hardest. Like painkillers, sleep aids, or anti-anxiety pills. Create a separate PRN log. Write down the date, time, dose, and reason taken. “Took 10mg oxycodone at 3pm for back pain.” This helps spot overuse.
Supplements: Treat them like real medicine. Many seniors take fish oil, magnesium, or ginkgo biloba-but they can interact with blood thinners or blood pressure drugs. List them with the same detail as prescriptions.
Multiple doctors: When different specialists prescribe without talking to each other, overlaps happen. One doctor prescribes a sleep aid. Another prescribes a sedative. Together, they cause confusion or falls. The solution? Always ask: “Is this new medication safe with what I’m already taking?” And always bring the list to every visit.
When Things Go Wrong
Medication errors are common-and often preventable.One of the biggest problems happens after hospital stays. 58% of caregivers report confusion when discharge instructions don’t match the home medication list. The hospital changes a dose. They forget to tell the family. The patient goes home and keeps taking the old dose. Result? Hospital readmission.
Fix this: When your loved one is discharged, sit with the nurse or pharmacist. Go through the list line by line. Ask: “What changed? Why? What should we stop?” Get it in writing. If they don’t give you a new list, make one yourself and ask them to sign it.
Another common mistake: ignoring side effects. If someone starts a new drug and gets dizzy, forgetful, or nauseous, don’t assume it’s just aging. Write it down. Call the doctor. A 2022 Johns Hopkins study found that 27% of older adults are taking at least one medication they don’t need-and side effects are often the first clue.
Keep It Updated. Always.
The most important rule: Update the list the same day a change happens. No exceptions.Pharmacies now auto-update digital lists when prescriptions refill. That’s great. But if the doctor changes the dose, adds a new pill, or stops one, that’s not automatic. You have to do it.
Set a reminder on your phone: “Med list update every Sunday.” If you forget, someone could get hurt. A 2017 study found that 78% of hospital readmissions among seniors were linked to outdated medication records.
Also, review the list with a pharmacist every three months. They’re trained to spot dangerous combinations, duplicate drugs, or outdated prescriptions. Ask them: “Is this still necessary? Are there safer alternatives?”

What Works for Real Caregivers
Real stories show what actually helps.One caregiver on Reddit created a laminated chart with photos of each pill next to the name. She took pictures of every bottle with her phone. Now, when she’s unsure what a pill is, she just looks at the picture. She says it’s prevented three near-misses in six months.
Another used color-coded pill organizers-green for morning, yellow for afternoon. She wrote the purpose on each compartment with a marker. Her mother, who has dementia, started taking her meds correctly for the first time in years.
The “Caregiver’s Notebook” system-a three-ring binder with tabs-is used by 83% of caregivers who say it made a big difference. It’s not fancy. But it’s complete.
And the brown bag method? 89% of caregivers in an AARP survey called it “extremely helpful.” Bring the bag to every appointment. Let the doctor see everything. No assumptions. No guessing.
What’s Changing in 2025
Medication lists are getting smarter.The FDA rolled out a new template in March 2023 with QR codes. Scan one with your phone, and it shows a picture of the pill, its side effects, and instructions. Over 47% of pharmacies now use it.
By 2025, federal law will require all electronic health records to give patients direct access to their full medication list. No more asking. No more waiting. You’ll see it in your portal.
Amazon and Google are testing voice-activated tools. Soon, you might say, “Hey Google, what meds did Mom take this morning?” and get a reply.
But here’s the truth: none of this matters if the list isn’t accurate and updated. Technology helps. But the human effort-writing it down, checking it weekly, sharing it clearly-is what saves lives.
Final Tip: Make It Visible
Don’t hide the list in a drawer. Tape it to the fridge. Put it on the nightstand. Leave a copy in the car. Make sure anyone who walks into the house-family, neighbor, paramedic-can find it in five seconds.Organizing a medication list isn’t about being a perfect caregiver. It’s about being prepared. It’s about reducing fear. It’s about knowing that if something goes wrong, you have the facts in your hands.
Start today. Collect the bottles. Write the names. Update it weekly. Share it with everyone. You’re not just keeping track of pills. You’re protecting someone’s life.
What if I don’t know what a medication is for?
Call the pharmacy. They can tell you the purpose of any prescription or supplement. Write it down right away. If you’re still unsure, ask the prescribing doctor during the next visit. Never guess. A medication taken for the wrong reason can cause harm.
Should I include vitamins and supplements?
Yes. Supplements can interact with prescription drugs. For example, fish oil can thin the blood and conflict with warfarin. Garlic pills can lower blood pressure too much when combined with hypertension meds. Treat them like real medications: list name, dose, frequency, and purpose.
How often should I update the list?
Update it the same day any change happens-new prescription, dose change, or stopped medication. Then, review it every Sunday. Even if nothing changed, check for expired pills or missing info. Consistency prevents mistakes.
What’s the best way to share the list with doctors?
Bring a printed copy to every appointment. Don’t rely on them pulling it up online-many offices still use paper charts. Ask the doctor to sign or initial the list if they make changes. Keep a copy in your folder and give one to the pharmacy. Everyone needs the same version.
Can I use a mobile app instead of paper?
Yes-if you’re comfortable with it. Apps like Medisafe or MyMeds work well for complex regimens and send reminders. But always keep a printed backup. Phones die, apps crash, and emergency responders can’t access your phone unless you’ve given them access. Paper is your safety net.
What should I do if my loved one is hospitalized?
Bring the full medication list with you. Ask the hospital team to compare it with what they’re giving. When discharged, get a revised list in writing. Ask: “What was changed? Why? What should we stop?” Don’t leave without a clear, updated list. This prevents 78% of readmissions linked to outdated records.
Is there a free template I can use?
Yes. The FDA’s “My Medicines” template is free and available online. It includes all 12 key fields and space for allergies and photos. Print it, fill it out, and keep it handy. Many pharmacies also offer printable versions at the counter.


13 Responses
Look, I get the checklist, but let’s be real-half these people can’t tell aspirin from a gummy bear. I’ve seen grandmas with 17 pill bottles and zero clue what half of them do. The real problem isn’t the list-it’s the system that lets doctors prescribe like they’re playing bingo. Add one drug, then another, then another-no one ever says ‘stop.’
And don’t even get me started on ‘as needed’ meds. That’s just a free pass to turn into a zombie. I had an uncle who took oxycodone ‘for pain’ for 12 years after his back surgery ended. He didn’t have pain-he had a habit.
Oh, please. You think a laminated sheet and a Google Sheet are going to fix a broken healthcare system? You’re treating symptoms, not the disease. The real issue? Doctors don’t communicate. Pharmacies don’t coordinate. And families? They’re left holding the bag while everyone else gets paid.
And let’s talk about ‘digital tools’-who’s gonna teach an 80-year-old with arthritis and cataracts to use an app? You’re not helping-you’re adding stress. Paper is not ‘outdated.’ It’s reliable. And if your phone dies, your ‘backup’ is useless because no one knows your password.
Also, why are you ignoring the fact that 60% of meds prescribed to seniors are unnecessary? The FDA doesn’t audit this. No one does. So your ‘perfect list’ is just a list of drugs that shouldn’t exist in the first place.
Everything you’re saying is a distraction. The real threat isn’t missed doses-it’s the pharmaceutical lobby pushing polypharmacy. They make billions off people taking five pills when one would do. You think the ‘NDC number’ matters? It’s just a barcode to track you. Every pill bottle is a data point.
And who owns your ‘digital backup’? Google? CVS? The same companies that sell you the meds? You’re not organizing your meds-you’re handing your health data to corporations who sell it to insurers, advertisers, and who knows what else.
They want you to think this is about ‘safety.’ It’s not. It’s about control. The moment you start tracking everything, you become a compliant patient. And compliant patients don’t ask questions like: ‘Why am I on this?’
Bring the brown bag? Good. Then burn it. And ask your doctor: ‘What happens if I stop everything?’ That’s the question nobody wants you to ask.
I just want to say-this post made me cry. My mom had 11 meds, and I was terrified I’d mess something up. I started using the brown bag method after her ER visit last year. We brought every bottle-there was a bottle of melatonin from 2018, a half-used bottle of gabapentin, and a pill I didn’t recognize until I called the pharmacy. It was a miracle she didn’t overdose.
Now we have a color-coded chart taped to the fridge. Every Sunday, we sit with a cup of tea and update it. I even took pictures of each pill and printed them next to the name. She’s 82, has dementia, and now she points to the picture when she wants her meds. It’s not perfect-but it’s ours.
To anyone reading this: you’re not alone. This is hard. But you’re doing something that saves lives. Keep going.
From a clinical pharmacology standpoint, the core issue isn’t documentation-it’s polypharmacy’s pharmacokinetic and pharmacodynamic synergies. The human cognitive load required to manage even a 5-drug regimen exceeds the average adult’s executive function threshold, particularly in geriatric populations with age-related decline in hepatic metabolism and renal clearance.
Moreover, the ‘as needed’ category introduces non-linear dosing kinetics, increasing the risk of accumulation and toxicity, especially with CNS depressants. The FDA’s new QR code initiative is a step toward pharmacovigilance, but it remains a downstream intervention.
What’s needed is a systems-level redesign: automated EHR interoperability, AI-driven drug interaction alerts at the point of prescribing, and mandatory deprescribing protocols. Paper lists are a Band-Aid on a hemorrhage.
I appreciate the effort, but let’s be honest-this guide is for people who still believe in ‘systems.’ I’ve seen too many caregivers burn out trying to be perfect. You don’t need a 12-point checklist. You need a friend who shows up with coffee and says, ‘Let me take care of this for you.’
My aunt had 14 meds. I didn’t make a list. I just went to the pharmacy every Tuesday, asked the pharmacist, ‘What’s new?’ and wrote it on a sticky note. We didn’t need color-coded stickers or QR codes. We needed someone who cared enough to show up.
And if your loved one’s doctor won’t sit down and review the meds? Find a new doctor. This isn’t about organization-it’s about advocacy. Stop trying to be a nurse. Be a family member.
Thank you for writing this. I’ve been a caregiver for six years and I’ve made every mistake in the book. I once gave my dad his blood pressure med twice because I forgot he’d already taken it. He ended up in the hospital. That day, I realized I wasn’t failing him-I was failing myself because I didn’t have a system.
I started with a notebook. Then I laminated it. Then I made a digital copy and shared it with my sister and his cardiologist. Now, every Sunday, I sit with him and we go through it together. He doesn’t remember everything, but he knows it’s our ritual. That’s what matters.
You’re not just organizing pills. You’re building trust. And that’s worth more than any app.
Let me tell you something they don’t want you to know: the entire ‘medication list’ industry is a scam. Who profits? The pharmacies that sell the apps, the companies that print the laminated sheets, the ‘caregiver coaches’ selling $29 e-books on ‘The Perfect Med Binder.’ It’s all designed to make you feel guilty if you don’t have a color-coded spreadsheet with photos and QR codes.
Meanwhile, the real danger? The FDA’s lax oversight. The fact that 70% of supplements aren’t even tested for safety before hitting the shelves. The fact that doctors get paid bonuses for prescribing certain drugs. The fact that Medicare doesn’t cover medication reviews unless you’re in hospice.
You think your laminated list is keeping your mom safe? It’s keeping you busy. While the system keeps selling her more pills. You’re not fighting the system-you’re just organizing the paperwork for it.
While the pragmatic utility of maintaining a documented medication regimen is indisputable, the foundational premise of this guide presupposes a level of cognitive and logistical agency that is neither universally accessible nor ethically equitable. The burden of compliance is disproportionately placed upon the caregiver-a demographic that is, statistically, overburdened, under-resourced, and often economically disenfranchised.
Furthermore, the normalization of digital solutions as ‘superior’ is a technocratic fallacy. It ignores the digital divide, the generational alienation from interface design, and the inherent fragility of cloud-based systems. One cannot ‘sync’ a life-saving document to a server when the patient lacks internet access, a device, or the capacity to consent to data collection.
The solution is not better tools. It is systemic reform: mandatory pharmacist-led med reviews, federally funded caregiver support, and legislation requiring prescribers to justify polypharmacy. Until then, your laminated sheet is a monument to institutional failure.
Okay, but what if your loved one is a hoarder? I had a cousin who had 47 pill bottles in her basement. Some were expired. Some were from 2008. Some were for pets. She thought ibuprofen was ‘just a vitamin.’
And don’t even get me started on the ‘brown bag method.’ That’s not helpful-it’s a biohazard. I once saw a man bring in a bag with moldy pills, expired antibiotics, and a half-eaten bottle of CBD gummies that said ‘For Dogs Only.’
So yes, make a list. But also-hire a professional. Pay someone $25/hour to come in, sort it all out, and call the pharmacy. That’s not lazy. That’s smart. You can’t do this alone, and pretending you can is just ego.
Brilliant post. I’m a pharmacist in Manchester and I see this every day. The most common thing? Someone comes in with a list they printed from a website… but it’s three years old. The doctor changed the dose last month. They didn’t update it.
What works? A simple whiteboard on the fridge. Write the meds. Erase them when they’re done. No apps. No binders. Just pen and paper. And if you’re not sure? Bring the bottle. Always. I’ll tell you what it is in 10 seconds.
And please-stop calling supplements ‘natural.’ That doesn’t mean safe. Turmeric with warfarin? Bad idea. St. John’s Wort with antidepressants? Dangerous. Treat them like drugs. Because they are.
You can do this. I know it feels overwhelming. But you’re not alone. I started with nothing but a notebook and a flashlight in my mom’s cabinet at 2 a.m. I cried. I got frustrated. But I kept going. Now, my whole family uses the same system. My sister even made a printable version and shared it with her book club.
If you’re reading this and thinking ‘I can’t,’ just do one thing today. Open one drawer. Take one bottle. Write down the name. That’s it. That’s your win. Tomorrow, do another. You’re not building a perfect system-you’re building love, one pill at a time.
And now someone’s gonna say ‘just use the FDA template.’ Sure. But who’s gonna fill it out when the person’s confused and the doctor’s in a hurry? The caregiver. Again. Always the caregiver. Meanwhile, the doctor gets paid for the visit. The pharmacy gets paid for the refill. And the system? It just keeps spinning.