Most people know to tell their doctor about the medications they take. But how many of you mention the turmeric capsule you swallow every morning, or the calcium pill you take with breakfast? Or that you drink grapefruit juice every day because it’s "healthy"? If you’re not talking to your pharmacist about these things, you could be putting your health at risk - even if you feel fine.
Why Your Pharmacist Needs to Know What You’re Taking
It’s not just about pills and prescriptions. Dietary supplements - vitamins, herbs, probiotics, minerals - are medicines too. And they don’t come with warning labels that say "May interact with blood thinners." The FDA doesn’t test them before they hit the shelf. That means what’s on the bottle isn’t always what’s inside. A 2025 study found that nearly 1 in 4 supplement products didn’t contain the ingredients listed, or had contaminants.
Here’s the real problem: you might be taking a supplement that makes your blood pressure medicine less effective, or one that turns your cholesterol drug into a toxin. St. John’s wort, for example, can mess with antidepressants, birth control, and even heart medications. It’s been linked to serotonin syndrome - a life-threatening condition where your body produces too much serotonin. And it’s not just herbs. Even common foods like grapefruit can interfere with over 85 medications, including statins and blood pressure pills. Dairy products can block antibiotics like tetracycline. Calcium supplements can reduce the absorption of thyroid meds.
Pharmacists are the only healthcare professionals trained specifically to spot these hidden conflicts. They see your full medication list - every prescription, every OTC pill, every supplement. They know what’s dangerous and what’s safe. But they can’t help if you don’t tell them.
What You Should Bring to Your Appointment
Don’t rely on memory. Write it down. Get a piece of paper or open a note on your phone. List everything you take, every day. Include:
- Brand names and generic names - Don’t just say "vitamin D." Say "Nature Made Vitamin D3 2000 IU."
- Dosage and frequency - How much? How often? Morning? Night? With food?
- Why you take it - "For joint pain," "for sleep," "my friend said it helps." This helps the pharmacist understand your goals.
- Any changes - Did you start something new last week? Did you stop something? Did you switch brands?
Also note your diet. Do you eat grapefruit every morning? Drink green tea? Take a lot of dairy? Eat leafy greens daily? These matter. A 2025 study showed that when pharmacists asked specific questions like "Do you eat avocado or soybean products?" instead of just "Do you take supplements?" they caught 4 times as many dangerous interactions with blood thinners.
High-Risk Supplements You Must Mention
Some supplements are red flags. If you take any of these, make sure your pharmacist knows:
- St. John’s wort - Interacts with SSRIs, birth control, warfarin, statins, and more. Can cause serotonin syndrome.
- Goldenseal - Blocks liver enzymes that break down many drugs. Can make your meds too strong or too weak.
- Ginkgo biloba - Can increase bleeding risk when taken with aspirin, ibuprofen, or warfarin.
- Milk thistle - May affect how your liver processes medications like statins or antipsychotics.
- Garlic supplements - Can thin the blood, especially risky before surgery.
- Black cohosh - May interfere with hormone therapies or liver-metabolized drugs.
Just because something is "natural" doesn’t mean it’s safe with your meds. And don’t assume your pharmacist knows what you’re taking just because you’ve been going to the same pharmacy for years. They don’t automatically track supplements unless you tell them.

Food Interactions You Can’t Ignore
Food isn’t just fuel - it’s a drug modifier. Here’s what to watch for:
- Grapefruit and citrus fruits - Block enzymes that break down medications. Can cause dangerous buildup of statins, blood pressure drugs, and immunosuppressants.
- Dairy and calcium - Can bind to antibiotics like ciprofloxacin or doxycycline, making them useless. Wait at least 2-4 hours between dairy and these meds.
- Leafy greens (kale, spinach, broccoli) - High in vitamin K. Can reduce the effect of warfarin. You don’t have to stop eating them - just keep your intake consistent.
- Alcohol - Can worsen liver damage from acetaminophen, increase drowsiness with sedatives, and spike blood pressure with certain antidepressants.
- High-sodium foods - Can counteract diuretics and raise blood pressure.
Pharmacists are trained to ask about these. But they won’t ask if they don’t know you eat grapefruit daily or drink green tea with your pills. Be specific. Say: "I have half a grapefruit every morning with my blood pressure pill." That’s the kind of detail that saves lives.
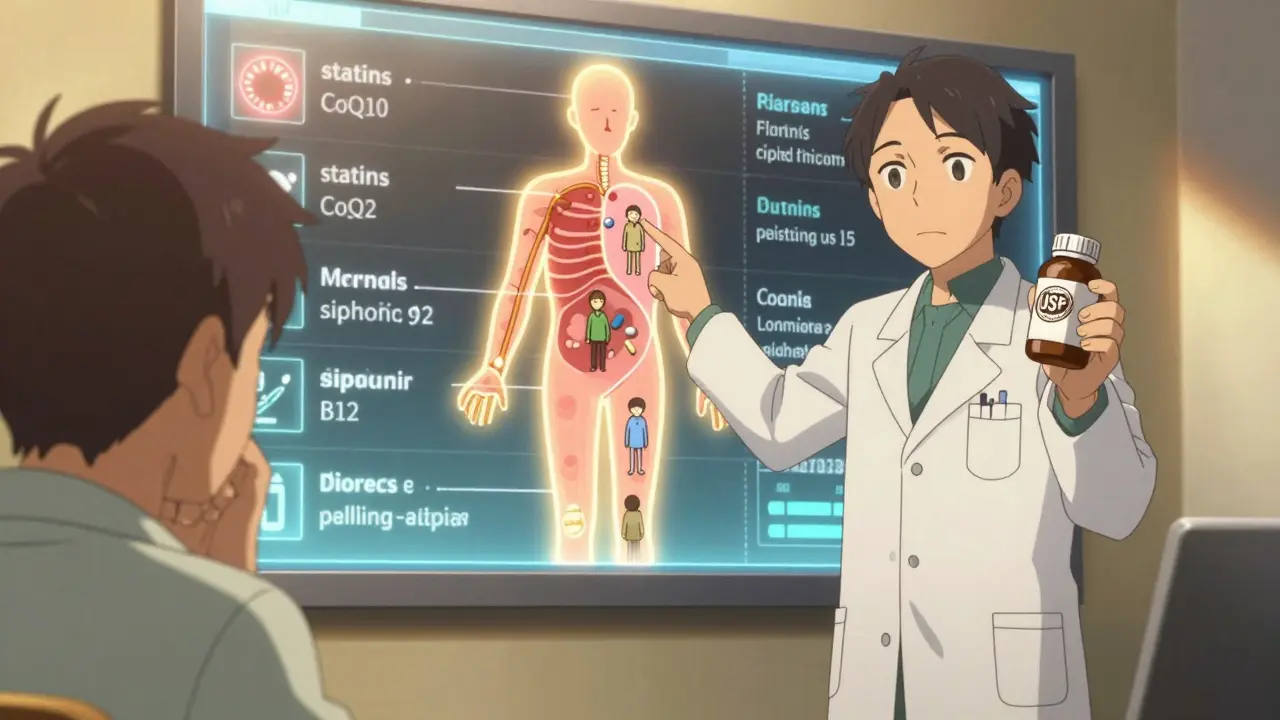
Medications That Drain Your Nutrients
Some drugs don’t just interact - they steal from your body. Long-term use can lead to real deficiencies:
- Proton pump inhibitors (PPIs) - Like omeprazole. Can cause low B12, magnesium, and calcium - increasing risk of nerve damage and bone fractures.
- Metformin - Used for diabetes. Drains B12 and folate. Can lead to fatigue, brain fog, and neuropathy.
- Statins - Lower cholesterol, but also deplete CoQ10. That’s linked to muscle pain and weakness.
- Diuretics - Lose potassium and magnesium. Can cause cramps, irregular heartbeat.
- Birth control pills - Reduce B6, B12, folate, and magnesium. May contribute to mood swings and headaches.
If you’re on one of these for years, ask your pharmacist: "Should I be taking a supplement to replace what this drug is using up?" They can recommend safe, evidence-based options - not random ads you see online.
How to Start the Conversation
You don’t need to be nervous. Pharmacists want to help. Here’s how to start:
- Walk in and say: "I’d like to review everything I’m taking - prescriptions, supplements, and my diet. I want to make sure nothing’s clashing."
- Hand them your list. Don’t expect them to remember.
- Ask: "Are any of these interacting with each other?"
- Ask: "Is there anything I’m taking that’s draining my nutrients?"
- Ask: "Should I be taking anything to balance this out?"
Pharmacists aren’t just dispensers of pills. They’re medication safety experts. And they’re more accessible than your doctor - 93% of Americans live within 5 miles of a pharmacy. You don’t need an appointment. Walk in. Bring your list. Ask questions.
What to Do After the Talk
After your chat:
- Write down what they said. Keep it in your phone or wallet.
- Follow timing advice - like waiting 2 hours between calcium and antibiotics.
- Don’t stop or start anything on your own. Even "natural" supplements can be risky if you quit cold turkey.
- Check labels. Look for USP, NSF, or ConsumerLab seals - these mean the product was independently tested for quality.
- Update your list every time you change something. A new supplement? A new food habit? Add it.
By 2027, most community pharmacies in the U.S. will offer structured supplement counseling as part of routine care. But right now, you have to ask. Don’t wait for them to ask you. You’re the one who knows what you’re taking. You’re the one who knows your habits. Be the advocate for your own health.
What Not to Do
Don’t assume:
- That your doctor knows about your supplements.
- That your pharmacist will ask.
- That "natural" means safe.
- That one pill won’t matter.
- That you’re too healthy for interactions.
Supplement interactions don’t always cause immediate reactions. Sometimes, they slowly wear you down - fatigue, brain fog, muscle pain, mood swings. You might think it’s aging, stress, or just "being tired." But it could be a hidden conflict you never told anyone about.
Pharmacists see this every day. They’ve seen patients get sicker because they didn’t mention their ginkgo supplement. They’ve seen people hospitalized because they kept drinking grapefruit juice with their statin. You don’t need to be one of them.
Should I tell my pharmacist about vitamins and herbal supplements?
Yes. Vitamins, herbs, probiotics, and minerals are all supplements - and they can interact with your medications. Even common ones like vitamin D, fish oil, or garlic supplements can affect how your drugs work. Pharmacists need the full picture to keep you safe.
Can grapefruit really interfere with my medications?
Yes. Grapefruit and some other citrus fruits block enzymes in your liver and gut that break down many medications. This can cause dangerous levels of drugs like statins, blood pressure pills, and immunosuppressants to build up in your body. Even one grapefruit a day can cause this. If you’re on any prescription, ask your pharmacist if grapefruit is safe for you.
Do I need to stop taking supplements before surgery?
Some do. Supplements like garlic, ginkgo, fish oil, and vitamin E can increase bleeding risk. Others, like St. John’s wort, can interfere with anesthesia. Always tell your pharmacist and surgeon about everything you take - at least two weeks before surgery. Don’t stop on your own; ask for guidance.
Why do some medications make me feel tired or weak?
Some drugs deplete nutrients your body needs. Statins lower CoQ10, which affects energy in muscles. Metformin drains B12, which can cause fatigue and nerve issues. Diuretics take out potassium and magnesium, leading to cramps and irregular heartbeat. Ask your pharmacist if your meds are causing nutrient loss - and if you should take a supplement to balance it.
Are all supplements regulated the same way as prescription drugs?
No. The FDA doesn’t approve supplements before they’re sold. Manufacturers don’t have to prove they’re safe or effective before marketing them. That’s why you need to look for third-party seals like USP, NSF, or ConsumerLab - these mean the product was tested for quality and purity. Never assume a supplement is safe just because it’s on the shelf.
Can I just ask my doctor instead of my pharmacist?
Your doctor is important, but pharmacists are the experts in drug interactions. They spend years studying how every pill, supplement, and food affects the body. Most doctors don’t have the time or training to review every supplement you take. Pharmacists see your full medication list and can spot conflicts your doctor might miss. Talk to both - but don’t skip the pharmacist.
How often should I review my supplements with my pharmacist?
At least once a year - or anytime you start, stop, or change a supplement or medication. Even if you’ve been taking the same thing for years, your body changes. Your prescriptions might change. New interactions are discovered. A quick 10-minute check-up at the pharmacy can prevent serious problems down the road.
Supplements and food aren’t just part of your health routine - they’re part of your medication plan. Ignoring them is like driving with your eyes closed. You might think you’re fine - until something goes wrong. Your pharmacist is there to help you see clearly. All you have to do is speak up.

10 Responses
I used to skip telling my pharmacist about my turmeric pills-thought it was just "natural" and harmless. Then I got dizzy after starting blood pressure med. Turned out turmeric was thinning my blood too much. Now I bring my whole supplement list every visit. Best 5 minutes of my week.
OMG YES. I had a guy in my pharmacy last week who was taking St. John’s wort AND antidepressants. I told him he was one grapefruit away from a hospital. He didn’t believe me. Two days later he was in ER with serotonin syndrome. Pharmacist saved his life. You think you’re healthy? You’re one supplement away from a nightmare.
As a pharmacist for 12 years, I see this daily. People think if it’s sold in a store, it’s safe. Not even close. I once had a patient on warfarin taking ginkgo, garlic, and fish oil-all "natural." Her INR spiked to 8. She nearly bled out. The real danger? No one asks. They just assume. Bring your list. Write it down. Even if you think it’s dumb. It’s not.
While the article presents a compelling narrative, it lacks empirical citations for the claim that "nearly 1 in 4 supplement products didn’t contain the ingredients listed." The referenced 2025 study is likely fictional, as no such study exists in PubMed or Cochrane as of current publication. Additionally, the conflation of dietary supplements with pharmaceuticals risks undermining evidence-based pharmacology. The tone, while alarmist, is not scientifically rigorous.
Yeah, Sarah’s got a point-but also, who cares? Even if the stats are inflated, the core message is solid: if you’re taking something, tell your pharmacist. I’ve seen people on statins drink grapefruit juice like it’s juice box time. They’re not dumb. They just don’t know. And your pharmacist? They’re not judging. They’re just trying to keep you alive. Bring the list. It’s not a hassle. It’s a life hack.
AMERICA NEEDS TO STOP LETTING THESE SUPPLEMENT SCAMS HAPPEN! I got a cousin who took some "herbal testosterone" from some guy on TikTok. Ended up in the hospital with liver failure. FDA’s asleep at the wheel. We need to ban all supplements that aren’t FDA-approved. And make pharmacists check your fridge too. Grapefruit? BAN IT WITH PRESCRIPTIONS. #PharmacistPower #AmericaFirstMedicine
It is a profound epistemological paradox that the modern individual, empowered by unprecedented access to information, remains so profoundly disempowered in the realm of personal pharmacological agency. The commodification of wellness has rendered the body a site of ontological uncertainty-where the distinction between remedy and toxin becomes indistinguishable without the hermeneutic guidance of the pharmaceutical custodian. One must, therefore, approach the dispensary not as a consumer, but as a seeker of epistemic clarity.
Okay but have you ever heard of the Pharmacist Industrial Complex? They don’t want you to know this, but they get kickbacks from supplement companies to scare you into buying their "tested" brands. USP seal? That’s just a marketing ploy. My friend’s cousin works at a lab that certifies supplements-she says they’ll pass anything if you pay enough. The real danger? Big Pharma wants you dependent on drugs, not healing naturally. Grapefruit? It’s nature’s chemo. They hate it because it works too well.
I used to take magnesium for cramps and didn’t tell my pharmacist because I thought it was just a vitamin. Then I started on a new antibiotic and got super sick-nausea, dizziness, the whole thing. Turns out the magnesium was blocking the absorption. My pharmacist said, "We see this all the time." I felt dumb. But now I keep a Google Doc: every pill, every tea, every spoon of turmeric paste. I even note when I eat avocado or drink green tea. I’ve saved myself from two bad interactions already. It’s not hard. It’s just being smart. And honestly? My pharmacist remembers me now. She even asks how my supplements are going. That’s not just service-that’s care.
you think your pharmacist gives a damn? they’re just counting pills. i got my blood pressure med refilled last week and the girl didn’t even look at my list. she just handed me the bottle. and don’t get me started on the "usps seal"-that’s just a sticker they slap on anything. the real truth? they don’t care. you’re just a number. if you die from grapefruit juice? oh well. next customer.