Every year, Americans spend over $650 billion on prescription drugs. That’s more than any other country in the world. But here’s the surprising part: generics make up 90% of all prescriptions filled - yet they account for only 12% of the total cost. Meanwhile, brand-name drugs, which are prescribed just 10% of the time, eat up 88% of the spending. This isn’t a glitch. It’s the power of generic medications at work.
What Exactly Are Generic Drugs?
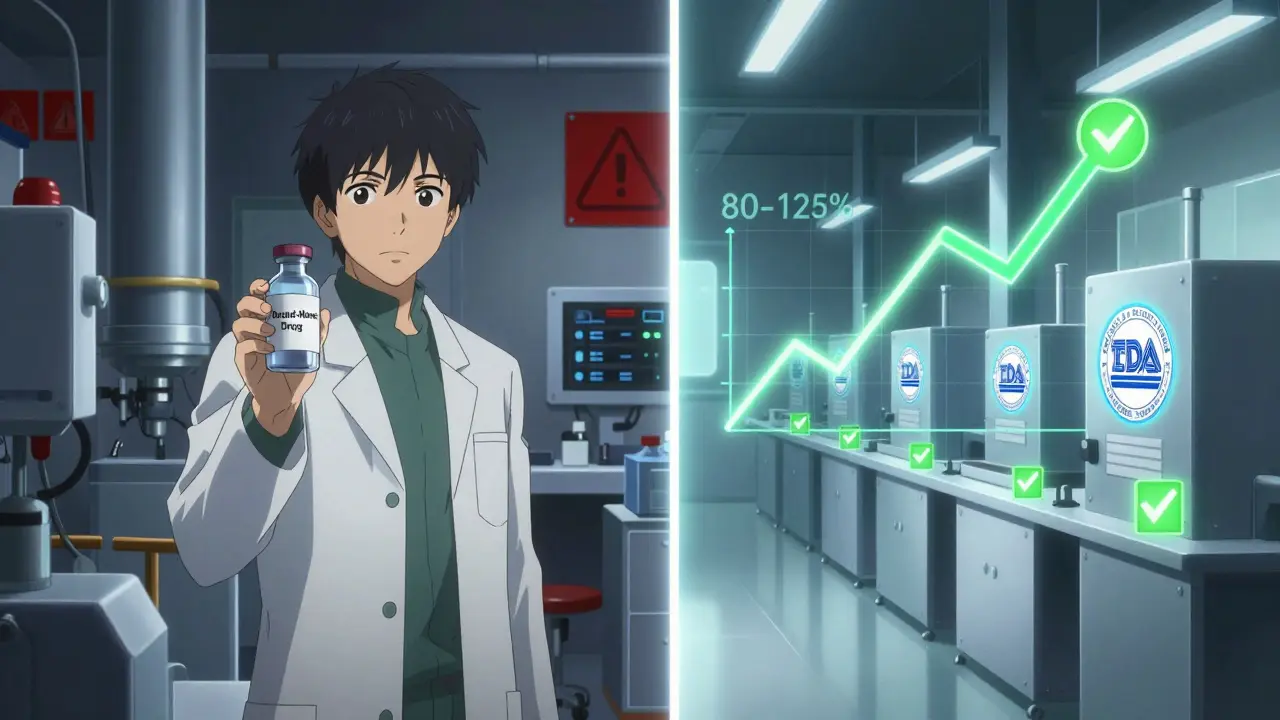
Generic drugs aren’t cheap knockoffs. They’re exact copies of brand-name medications, approved by the FDA after the original patent expires. The active ingredient, dosage, strength, and how it works in your body are identical. The only differences? The color, shape, or inactive ingredients like fillers - and the price. Generics typically cost 80-85% less than their brand-name equivalents.The legal backbone of this system is the Hatch-Waxman Act of 1984. Before that, companies had to run full clinical trials to prove a new drug was safe and effective - even if it was just copying an existing one. Hatch-Waxman changed that. It created a faster, cheaper path called the Abbreviated New Drug Application (ANDA). Now, manufacturers only need to prove their version is bioequivalent - meaning it behaves the same way in the body as the original.
To prove bioequivalence, companies test the drug in 24 to 36 healthy volunteers. Blood samples are taken over 72 hours to measure how much of the drug enters the bloodstream and how fast it’s absorbed. The FDA requires that the generic’s absorption rate falls within 80-125% of the brand-name drug. That’s not a wide range - it’s tight enough to ensure safety and effectiveness.
The Numbers Don’t Lie: Generics Save Billions
In 2024, Americans filled 3.9 billion generic prescriptions. That’s nearly 4 billion times someone chose a cheaper, equally effective option. The total cost for all those prescriptions? Just $98 billion. Meanwhile, the 435 million brand-name prescriptions cost $700 billion. That’s a 7-fold difference in spending for just one-tenth the volume.Since 2000, generics have saved the U.S. healthcare system over $445 billion. In 2024 alone, that number grew again. The Congressional Budget Office found that when a generic enters the market, prices drop by about 90% within a year. Compare that to Medicare drug price negotiations, which only cut prices by 42% on average. Generics don’t need legislation - they work the moment the patent expires.
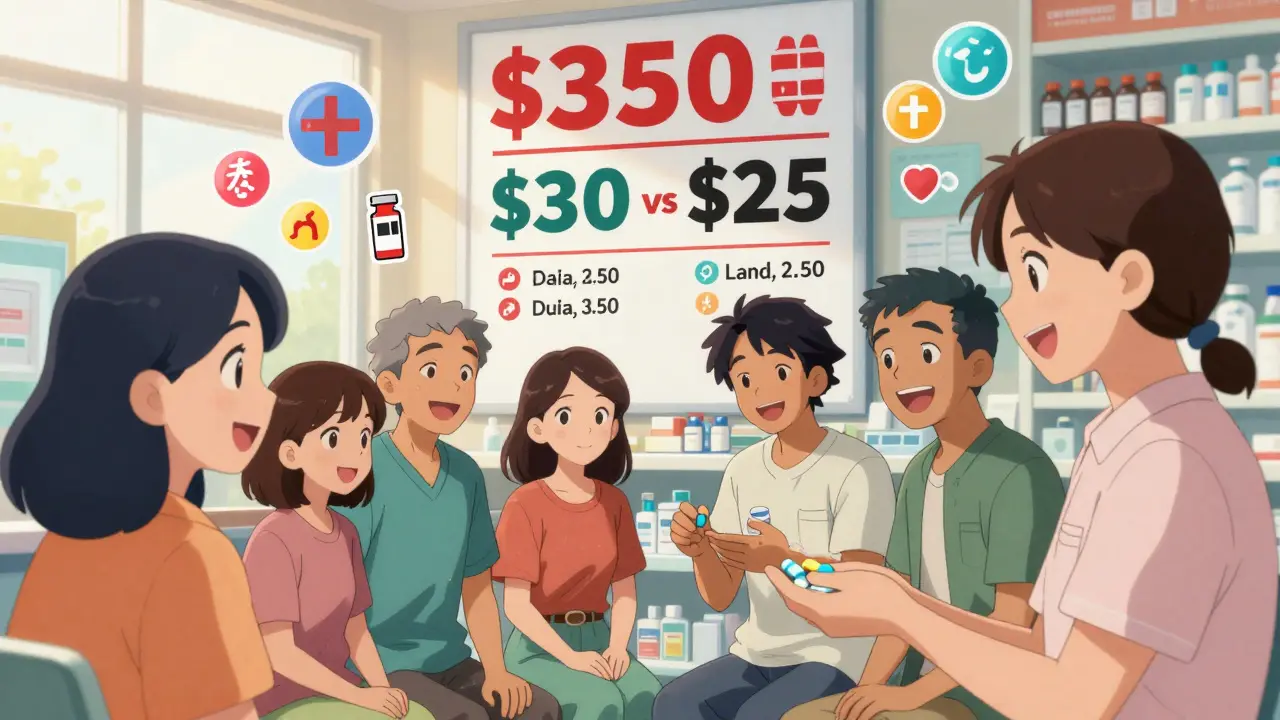
Take insulin, for example. Before 2023, Humalog cost over $350 a month, even with insurance. When generic insulin lispro became available, the price dropped to $25. Patients who once skipped doses to stretch their supply could now afford their treatment. That’s not just savings - that’s better health outcomes.
Why Aren’t All Drugs Generic?
Not every drug can be copied easily. Complex biologics - drugs made from living cells, like Humira or Enbrel - can’t be replicated exactly. That’s where biosimilars come in. These aren’t identical copies, but highly similar versions. They’re cheaper - usually 15-35% less than the brand - but still far more affordable than the original.Here’s the problem: only 10% of biologics have biosimilars available. Ninety percent of those set to lose patent protection in the next decade have no biosimilar in development. Why? Because biosimilars are expensive and complicated to make. The FDA’s approval process can take years. And even when approved, pharmacy benefit managers (PBMs) often push patients toward the original drug because of hidden rebates.
Then there’s the patent thicket. Brand-name companies file dozens - sometimes over 140 - patents on a single drug. These aren’t all about the medicine itself. They cover delivery systems, packaging, or minor formulation tweaks. Each patent can delay a generic entry by months or even years. One tactic, called “product hopping,” involves slightly changing the drug’s form (like switching from a pill to a capsule) to reset the patent clock. That’s legal - and it works.
Generics vs. Other Cost-Cutting Methods
There are other ways to control drug spending - but none work as fast or as broadly as generics.- Step therapy (forcing patients to try cheaper drugs first) saves about 12-15% per treatment episode - but only if patients stick with it.
- Value-based pricing (paying based on outcomes) has only shown 1-3% savings in pilot programs.
- Medicare negotiation could save $500 billion over 10 years - but only for 30 drugs a year, and only for Medicare patients.
Generics work for everyone. They don’t require changes to insurance rules or new laws. They’re automatic. When a patent expires, the market shifts. Price drops. Patients win.
Barriers to Wider Use
Even though generics are proven, safe, and cheap, they still face resistance.Some pharmacies charge higher copays for generics than brand-name drugs - yes, really. That’s because PBMs get bigger rebates from brand manufacturers. So even though the generic costs less, the patient pays more. In 2024, 45% of commercial insurance plans used this trick.
Doctors don’t always know when substitution is allowed. The FDA’s Orange Book lists which generics are interchangeable - but only 37% of physicians can correctly interpret the codes without checking. And in 12 states, pharmacists can’t switch a patient to a generic for drugs like warfarin or levothyroxine without the doctor’s permission - even if the FDA says it’s safe.
Then there’s the fear factor. Some patients report side effects after switching - nausea, dizziness, or rashes. Most of the time, it’s not the active ingredient. It’s the fillers. A 2023 FDA report logged over 1,200 adverse events linked to generic substitutions, mostly from changes in dyes or binders. For most people, it’s harmless. But for those with allergies or sensitivities, it matters.
Patients with narrow therapeutic index drugs - where tiny changes can cause big effects - are especially vulnerable. Levothyroxine, used for thyroid conditions, has a history of complaints. Some patients report symptoms returning after switching to a generic, even though bioequivalence tests say it’s fine. That’s why many doctors still prescribe the brand for these cases - not because generics are unsafe, but because the stakes are higher.

What’s Next for Generics?
The future of generics depends on three things: policy, manufacturing, and trust.The Inflation Reduction Act capped insulin at $35 a month for Medicare patients - and prices dropped across the board. That’s proof that regulation can force change. But it only applies to a handful of drugs. What we need is more pressure on patent abuse and faster approval for biosimilars.
Manufacturing is another issue. Over 80% of the active ingredients in U.S. drugs come from India and China. When supply chains broke down during the pandemic, over 300 drugs went into shortage - most of them generics. The FDA is now pushing for more domestic production, but it’s slow and expensive.
And trust? That’s the biggest hurdle. Patients need to know that a generic isn’t a second-rate option. A review of 1.2 million patient ratings on Drugs.com showed generics scored 4.1 out of 5 for effectiveness - almost identical to brand-name drugs. The only difference? Affordability. Generics scored 4.5 out of 5 for cost; brands scored a 2.3.
When people understand that, they choose generics. When they don’t, they pay more - and sometimes skip doses entirely. GoodRx found that 68% of patients who couldn’t afford brand-name drugs skipped or split pills. That’s not just a financial problem. It’s a public health crisis.
Final Thoughts
Generics aren’t a magic bullet, but they’re the most powerful tool we have to control drug spending. They work fast, they work for everyone, and they work without needing Congress to pass new laws every time.The real challenge isn’t science - it’s systems. Pharmacy benefit managers, patent lawyers, and outdated insurance rules are keeping prices high. We need transparency. We need enforcement. And we need patients to demand better.
For now, the message is simple: if your doctor prescribes a brand-name drug, ask if there’s a generic. If your pharmacist says it’s not available, ask why. And if you’re paying more than $25 for insulin, you’re being overcharged - and you have the right to know why.
Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Over 90% of generic drugs are rated as therapeutically equivalent by the FDA. Millions of patients use them safely every day.
Why are generics so much cheaper?
Generics don’t need to repeat expensive clinical trials. The original drug company already proved the drug works and is safe. Generic manufacturers only need to show their version behaves the same way in the body. That cuts development costs by 90%. They also don’t spend millions on advertising. Those savings get passed on to consumers.
Can I switch from a brand-name drug to a generic without my doctor’s approval?
In most cases, yes. Pharmacists are allowed to substitute generics unless the doctor writes "Dispense as Written" or "No Substitution" on the prescription. In 48 states, pharmacists can make the switch automatically. But for drugs with a narrow therapeutic index - like warfarin or levothyroxine - some states require the doctor’s permission, even if the FDA says it’s safe.
Why do some people say generics don’t work as well?
Most of the time, it’s not the drug - it’s the fillers. Generics can use different inactive ingredients like dyes or binders, which can cause mild side effects in sensitive people. In rare cases, patients with thyroid conditions or epilepsy report symptoms returning after switching. These are exceptions, not the rule. If you notice a change, talk to your doctor. You can always go back to the brand if needed.
What’s the difference between generics and biosimilars?
Generics are exact copies of small-molecule drugs - like pills for blood pressure or cholesterol. Biosimilars are similar - but not identical - to complex biologic drugs made from living cells, like insulin or rheumatoid arthritis treatments. Biosimilars are harder to make and cost more to develop, so they’re usually only 15-35% cheaper, not 80%. But they’re still a major step toward lowering costs for expensive treatments.
If you’re taking a brand-name drug, check your prescription label. Look up the generic name. Ask your pharmacist if a cheaper version is available. You might be surprised how much you can save - without giving up effectiveness.

11 Responses
Let’s be real - if you’re still skeptical about generics, you’re either paying for branding or you’ve been fed too much Big Pharma propaganda. The FDA doesn’t approve just anything, and bioequivalence isn’t some loophole - it’s a rigorous standard. I’ve been prescribing generics for 18 years. Zero compromise in efficacy. Zero. The only people who suffer are those who don’t ask for the cheaper option because they think ‘brand’ means ‘better.’ Spoiler: it doesn’t.
And don’t even get me started on PBMs gaming the system. They’re the real villains here - not generics. They make you pay more for a $25 drug because the brand paid them a kickback. It’s not just unethical - it’s criminal.
Meanwhile, patients skip doses because they can’t afford insulin. That’s not a policy failure. That’s a moral one. And we’re all complicit when we stay silent.
Actually, you’re all wrong. Generics aren’t safe. I had a cousin who went into seizures after switching from brand-name Lamictal to generic. Turned out the fillers triggered a reaction. The FDA’s 80-125% window? That’s a joke. One percent difference in absorption can be the difference between life and death for someone with epilepsy. You think it’s fine because you’re not the one vomiting blood or having a stroke? That’s not science - that’s luck.
And don’t tell me about savings. When your kid’s on a drug with a narrow therapeutic index, ‘savings’ means ‘dead kid.’
Thank you for writing this. I’ve been too scared to switch my levothyroxine because I’ve heard horror stories, but now I feel like I can ask my pharmacist without feeling like I’m being reckless. I didn’t realize generics scored 4.1/5 on effectiveness - that’s almost the same as brand. I’m going to ask for the generic next refill. If it works, I’m saving $120 a month. That’s my grocery budget.
Also - why do pharmacies charge more for generics? That makes zero sense. I’m calling my insurance tomorrow.
You’re right. We need to demand better. I’m done being guilted into paying more for nothing.
There’s a quiet revolution happening in pharmacy tech right now. Some independent pharmacies are starting to print out side-by-side comparison sheets for patients - showing the exact same active ingredient, bioequivalence data, and even the manufacturer’s lot numbers. It’s not flashy, but it’s working. Patients who see the data stop worrying.
And for the record - the 1,200 adverse events from fillers? Most were mild. Rash, headache. Nothing life-threatening. Compare that to the 2.7 million people who skip doses because they can’t afford the brand. That’s the real crisis.
Generics aren’t perfect. But they’re the closest thing we have to a free lunch in healthcare.
My husband died because he couldn’t afford his brand-name heart medication. He switched to the generic because he had no choice. They said it was fine. He died two weeks later. The coroner said it was cardiac arrest. But I know. He stopped taking it because he couldn’t afford it. The generic didn’t kill him. The system did.
So don’t lecture me about ‘savings.’ Some of us don’t get to choose between ‘safe’ and ‘cheap.’ We just get to choose between dying and living on crumbs.
Let’s cut through the virtue signaling. The real issue isn’t generics - it’s that the U.S. has the most broken pharmaceutical supply chain in the developed world. We outsource 80% of API production to China and India, then act shocked when there’s a shortage. We let patent trolls file 140 patents on one drug. We let PBMs control distribution. And then we blame patients for not knowing the difference between ‘bioequivalent’ and ‘identical.’
Generics are a band-aid on a hemorrhage. Fix the system, not the label.
Yall americans are so dumb. Why you pay 350 for insulin? In canada we pay 20. No joke. And we have universal healthcare. You think your system is great? You pay more for everything and get less. Even your generics are overpriced because of your stupid insurance crap. Fix your country before you lecture me on science.
For anyone scared to switch: if you’re on a drug with a narrow therapeutic index - levothyroxine, warfarin, phenytoin - talk to your doctor before switching. But here’s the truth: if you’ve been stable on the brand for years, switching might not be worth the risk. But if you’re new to the medication? Go generic. The data supports it.
And if you’re paying more for a generic than a brand? That’s not a mistake - that’s fraud. File a complaint with your state’s pharmacy board. They have to report PBM abuse.
Also - check Drugs.com. The ratings are real. Generics win on cost. Brands win on marketing. Choose wisely.
My mom is 78 and on six different meds. Five of them are generic. She’s been on them for 12 years. No issues. No hospitalizations. She saves $1,800 a year. That’s her heating bill. That’s her groceries. That’s her dignity.
I used to think generics were ‘lesser.’ Now I know they’re the quiet heroes of American healthcare. No fanfare. No ads. Just people getting better because they can afford to take their pills.
So if you’re reading this and you’re on a brand-name drug - ask. Just ask. You might be surprised.
As someone from India, I’ve seen generic manufacturing up close. The quality control is often better than in the U.S. - because the margins are so thin, they can’t afford mistakes. A single batch failure means bankruptcy. So they’re meticulous.
The problem isn’t the drug. It’s the middlemen. The PBMs, the insurers, the pharmacy chains - they’ve turned healthcare into a profit game. Generics are the only thing keeping it from collapsing.
And yes - the fillers matter. But so does not dying because you skipped your pill. Choose life. Choose the generic.
From a pharmacoeconomic standpoint, the cost-utility ratio of generic substitution is overwhelmingly favorable. The incremental cost-effectiveness ratio (ICER) for generic substitution across chronic conditions like HTN, DM2, and hyperlipidemia consistently falls below $5,000 per QALY gained - well below the WHO’s $150,000 threshold for cost-effective interventions.
Meanwhile, the structural barriers - patent evergreening, PBM rebate traps, and formulary non-interchangeability - represent market failures of the highest order. Regulatory capture is evident in the FDA’s delayed biosimilar approvals and the lack of transparency in PBM contracting.
Policy intervention must target these systemic inefficiencies rather than pathologizing patient behavior or stigmatizing generic use.