One glass of grapefruit juice in the morning might seem like a healthy start - until it turns into a silent danger if you’re on certain medications. This isn’t a myth or an old wives’ tale. It’s a well-documented, potentially life-threatening interaction that affects hundreds of thousands of people every year. The problem isn’t the sugar or the acidity. It’s something deeper, hidden in the fruit’s chemistry, that can turn your prescription into a poison.
What’s Really Happening in Your Body?
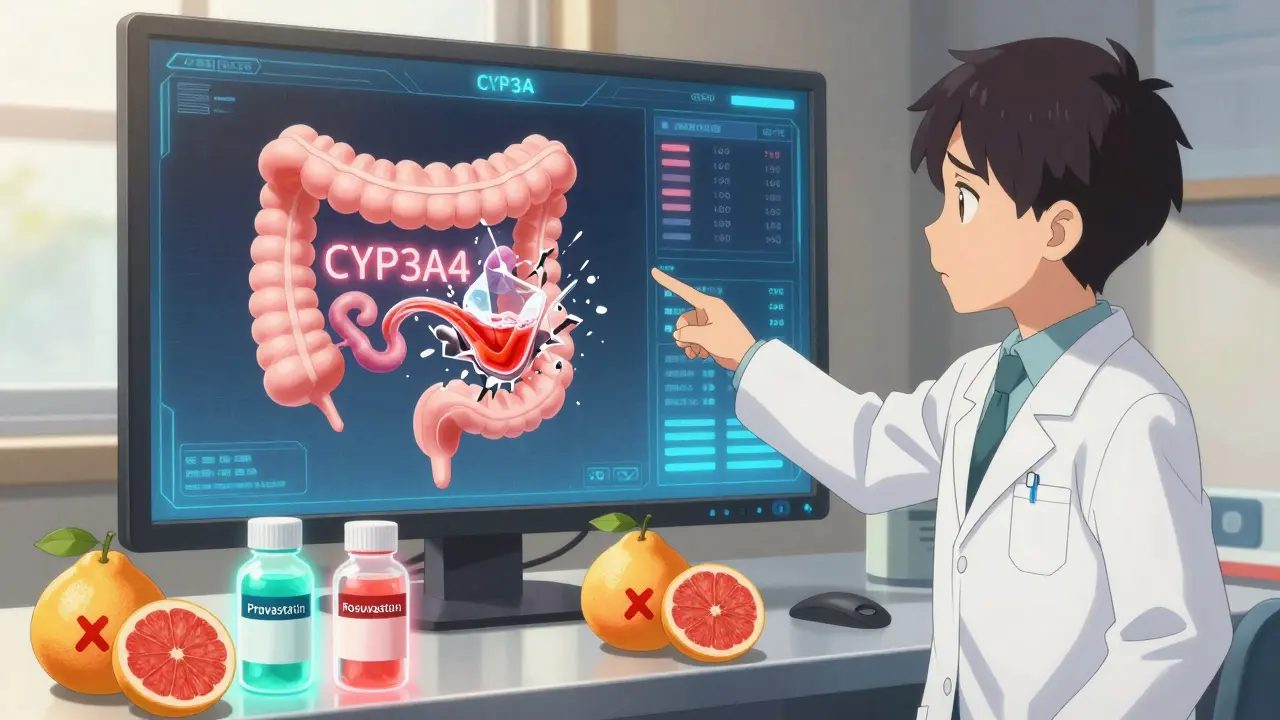
Grapefruit doesn’t just mix with drugs - it hijacks your body’s ability to process them. The culprit? Furanocoumarins, natural compounds found in grapefruit, Seville oranges, pomelos, and some limes. These chemicals don’t just pass through your system. They lock onto an enzyme in your gut called CYP3A4 and break it permanently. Think of CYP3A4 as a gatekeeper. It’s responsible for breaking down about half of all prescription drugs before they enter your bloodstream. When grapefruit knocks it out, those drugs flood into your body unchecked. This isn’t a temporary glitch. The enzyme doesn’t bounce back after a few hours. It takes days to regenerate. That means even if you take your pill at night and drink juice in the morning, you’re still at risk. The damage is done the moment you consume the fruit. One 200-milliliter glass - about six ounces - is enough to trigger this reaction. And it doesn’t matter if it’s fresh-squeezed, store-bought, or in a smoothie. All forms carry the same risk.Which Medications Are Most at Risk?
Not all drugs are affected equally. Some are barely touched. Others? They become dangerously potent. Here are the most common and dangerous categories:- Statins for cholesterol: Simvastatin (Zocor) is the worst offender. Drinking grapefruit juice while taking it can triple your blood levels. That raises your risk of rhabdomyolysis - a condition where muscle tissue breaks down, flooding your kidneys with toxic proteins. Lovastatin (Mevacor) and atorvastatin (Lipitor) are also risky, but pravastatin (Pravachol) and rosuvastatin (Crestor) are safe because they don’t rely on CYP3A4.
- Calcium channel blockers for blood pressure: Felodipine (Plendil), nifedipine (Procardia), and amlodipine (Norvasc) all spike in concentration. With felodipine, grapefruit juice can raise blood levels by more than 350%. That can lead to dangerously low blood pressure, dizziness, or even fainting.
- Immunosuppressants after transplants: Cyclosporine, tacrolimus, and sirolimus are critical for preventing organ rejection. Grapefruit can make their levels jump by 300% to over 1,100%. That doesn’t just mean more side effects - it means kidney failure, nerve damage, or life-threatening infections.
- Anti-anxiety and psychiatric drugs: Buspirone (Buspar) and sertraline (Zoloft) can build up in your system, increasing drowsiness, confusion, and heart rhythm problems.
- Blood thinners: Apixaban (Eliquis) and rivaroxaban (Xarelto) are safe, but warfarin (Coumadin) can become unpredictable. Grapefruit doesn’t directly interact with warfarin, but it can mess with other drugs you might be taking alongside it, making your INR levels swing dangerously.
The FDA has flagged 17 specific drugs with clear warnings on their labels. But there are 23 more where the risk is strong enough to be mentioned in prescribing guides. If your medication comes with a warning about grapefruit, don’t ignore it. Even if you’ve had juice for years without problems, your body changes. So do your meds.
Why Do Some People Get Hit Harder Than Others?
Not everyone reacts the same way. Genetics play a big role. Some people naturally have less CYP3A4 enzyme in their gut - meaning grapefruit hits them harder. A 2021 study found that people with a specific gene variant (CYP3A4*22) saw up to 40% higher drug levels after drinking grapefruit juice than those without it. Age matters too. People over 65 are more likely to be on multiple medications and more likely to drink grapefruit juice daily. The CDC says over half of older Americans take five or more prescriptions. That’s a perfect storm. Your liver health, your gut bacteria, even the time of day you take your meds - all these things can change how grapefruit affects you. That’s why there’s no safe amount. You can’t say, “I’ll just have half a glass.” You can’t wait three hours between juice and pills. The enzyme is gone. It won’t come back until your body makes new ones - and that takes days.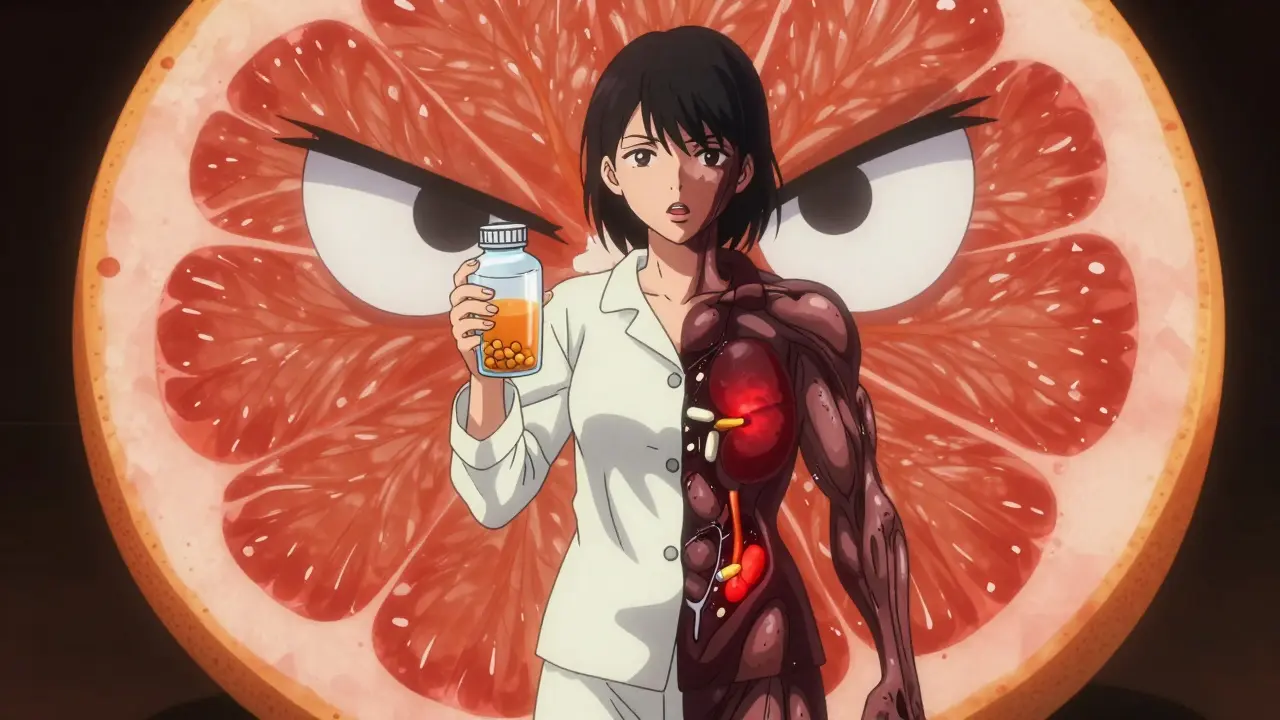
What About Other Citrus Fruits?
Don’t assume orange juice is safe just because it’s not grapefruit. Seville oranges - the kind used in traditional marmalade - contain the same furanocoumarins. Pomelos, which look like giant grapefruits, are just as dangerous. Even some limes, especially those used in juice blends, can trigger the same reaction. Sweet oranges (like navel or Valencia) and tangerines? They’re generally safe. But always check the label. Some juice blends mix in grapefruit or pomelo without saying so. And it’s not just citrus. One case report linked pomegranate juice to similar interactions. While it’s not as common, if you’re on a high-risk medication, it’s better to avoid it until you know for sure.What Can You Do Instead?
You don’t have to give up your morning routine. You just need to swap out the risky parts.- If you’re on simvastatin, ask your doctor about switching to pravastatin or rosuvastatin. Both work just as well and don’t interact with grapefruit.
- If you take amlodipine for blood pressure, diltiazem or verapamil might be safer alternatives.
- For blood thinners, apixaban or rivaroxaban are good options if you’re currently on warfarin.
Many of these alternatives are available as generics, so cost isn’t usually a barrier. Your pharmacist can help you compare options. In fact, 78% of community pharmacists in the U.S. now routinely check for grapefruit interactions during medication reviews. Don’t wait for them to ask - bring it up yourself.
What Should You Ask Your Doctor or Pharmacist?
Don’t leave this to guesswork. Use these three questions:- Does my specific medication interact with grapefruit or grapefruit juice?
- Is there a similar medication I can take that doesn’t have this risk?
- Are there other fruits, juices, or supplements I should avoid while taking this?
Write them down. Bring them to your next appointment. If your doctor says, “I don’t think it’s a big deal,” get a second opinion. This isn’t a minor warning. It’s a real, measurable risk that causes thousands of hospital visits every year. The FDA estimates grapefruit interactions lead to about 10,000 adverse events in the U.S. annually - many of them preventable.
What If You’ve Already Had Juice With Your Meds?
If you accidentally drank grapefruit juice with your medication, don’t panic. But don’t ignore it either. Watch for signs of overdose:- Unusual muscle pain or weakness (especially with statins)
- Severe dizziness or fainting (with blood pressure meds)
- Swelling in your legs or feet (sign of kidney strain)
- Extreme fatigue, confusion, or irregular heartbeat
If you notice any of these, call your doctor or go to urgent care. Don’t wait until tomorrow. The damage can start quickly, especially with immunosuppressants or statins.
Going forward, keep a list of your medications and the foods to avoid. Put it on your fridge. Share it with family members. Set a phone reminder: “No grapefruit today.” It’s not just about health - it’s about survival.
Is There Any Hope for the Future?
Scientists are working on solutions. Researchers are testing grapefruit varieties bred to have 85-90% less furanocoumarin. Early results are promising. But until those are widely available - and proven safe for every drug - the only guaranteed safety is avoidance.Electronic health records now flag grapefruit interactions automatically. Most hospitals in the U.S. have alerts built into their systems. That’s progress. But the real protection comes from you - knowing what’s in your cup, asking the right questions, and choosing safety over convenience.
There’s no shame in giving up grapefruit juice if it means staying out of the hospital. Your meds are meant to help you live longer, not shorten your life. And sometimes, the safest thing you can do is skip the fruit - even if it’s the one you love the most.
Can I drink grapefruit juice if I take my medication at night?
No. The enzymes in your gut that grapefruit disables take days to regenerate. Even if you take your pill at night and drink juice in the morning, the damage is already done. Timing doesn’t matter - only avoidance does.
Is orange juice safe to drink with medications?
Sweet orange juice - like navel or Valencia - is generally safe. But Seville oranges (used in marmalade), pomelos, and some limes are not. Always check the label on juice blends; some contain grapefruit or pomelo without listing it clearly.
Which statins are safe with grapefruit?
Pravastatin (Pravachol) and rosuvastatin (Crestor) are safe because they don’t rely on the CYP3A4 enzyme for metabolism. Simvastatin, lovastatin, and atorvastatin are not. If you’re on one of the risky ones, ask your doctor about switching.
How much grapefruit juice causes a reaction?
As little as 200 milliliters - about six ounces or one small glass - is enough to block CYP3A4 enzymes for up to 72 hours. There is no safe amount if you’re on a high-risk medication.
Can I eat grapefruit if I’m not on any medication?
Yes. Grapefruit is perfectly safe for people not taking medications that interact with it. It’s rich in vitamin C, fiber, and antioxidants. The risk only exists when it’s combined with certain drugs. If you’re unsure, check your medication labels or ask your pharmacist.
If you're managing multiple medications, keep a printed list in your wallet or phone. Include the drug name, dose, and any food restrictions. Share it with caregivers, family, or anyone who might help you in an emergency. Your health isn’t something to gamble with - even if it means giving up your favorite breakfast drink.


15 Responses
Bro, I drank grapefruit juice with my statin for 3 years and never felt a thing. Then one day my legs turned to jelly and I thought I was having a stroke. Turns out? My body finally said 'enough.' Now I drink orange juice and call it a win. Don't be that guy.
They say grapefruit is bad but what about the real enemy? Big Pharma. They don't want you to know that grapefruit is nature's way of saying 'your pill is overpriced junk.' They made these drugs to depend on broken enzymes so you'll keep buying them. Furanocoumarins? More like furanocoumarin-anti-corporate-warriors. Wake up.
It is with great respect for the scientific rigor presented herein that I acknowledge the profound implications of this interaction. In my own country, where polypharmacy is increasingly common among the elderly, this knowledge could be lifesaving. I shall share this with my aunt who takes cyclosporine after her transplant. Thank you for the clarity.
Just read this and immediately checked my meds. Turns out I'm on amlodipine. Holy crap. I drink grapefruit juice every morning. I'm calling my pharmacist right now. Thanks for the heads-up - this is the kind of info that actually saves lives.
Oh please. Americans are so dramatic. We've been drinking grapefruit juice with our meds for decades in the UK and nobody drops dead. You'd think the NHS would've banned it by now if it were that dangerous. Probably just another FDA scare tactic to sell more expensive alternatives.
grapefruit is a gmo plant created by big pharma to test if people are dumb enough to drink it with their pills. they want to see how many people die so they can charge more for the antidote. also the FDA is a puppet. dont trust anyone. i stopped eating everything after this.
So glad someone finally broke this down without jargon. I’m a nurse and I still get patients asking, ‘But I’ve had juice for 10 years!’ - yeah, and your kidneys are just waiting to throw a tantrum. Pro tip: If your med’s label says ‘avoid grapefruit,’ it’s not a suggestion. It’s a warning label. Like ‘do not put in microwave.’
Everyone’s acting like this is new. Newsflash: This has been known since the 90s. The reason it’s still a problem is because doctors don’t care. They write scripts and walk away. Pharmacists are the only ones who know, and they’re too busy counting pills to explain it. This isn’t science - it’s negligence.
I’m from the UK but my Indian cousin in Delhi just got a kidney transplant and she’s terrified she’ll mess up her meds. I printed this out and translated it into Hindi for her - she cried. Honestly, this is the kind of post that bridges cultures. Grapefruit might be a fruit, but this warning? It’s universal. Thank you for writing this with such care.
Just shared this with my dad. He’s on simvastatin and drinks grapefruit juice like it’s water. I sent him a meme of a grapefruit wearing a warning sign. He laughed… then Googled his med. He’s switching to pravastatin next week. You just saved his kidneys. 🙏
My mom takes blood pressure meds and loves her morning juice. I didn’t know this until today. We’re going to the grocery store tomorrow and swapping out the grapefruit for oranges. Simple fix, huge impact. Thanks for making it so clear.
💖 This is why I love Reddit. Someone takes the time to explain something life-or-death without being a know-it-all. I’m sharing this with my entire family. My grandma’s on cyclosporine and I had no idea. Now she’s getting a little ‘NO GRAPEFRUIT’ sticky note on her juice glass. 💪🍊🚫
Let me be brutally honest - this isn’t just about grapefruit. It’s about how broken our healthcare system is. People aren’t warned because doctors are overworked, pharmacists are understaffed, and patients are expected to read 12-page PDFs with 8-point font. This post should be mandatory reading for every new prescription. And yes, I’m sending this to my senator. If a fruit can kill you because no one bothered to tell you, that’s a systemic failure - not a personal mistake.
One of the most well-written, clinically accurate pieces I’ve read on this topic. The breakdown of CYP3A4, the distinction between statins, the emphasis on regeneration time - all spot on. I’m a physician assistant, and I wish every patient came in having read this. You’ve done the medical community a service. Thank you.
Interesting. I take rosuvastatin and drink grapefruit juice every day. I guess I am lucky. But I will still stop now, just to be safe. Better safe than sorry. Thank you for the information.