When you pick up a prescription, you might see two names on the bottle: one you recognize from TV ads, and another that looks completely different. The brand-name version costs $80. The generic? $12. You might wonder: is this cheaper version just as good? The short answer is yes - generic drugs are not inferior. They work the same way, in the same amount of time, with the same safety profile. But there’s more to it than just price.
What Makes a Drug ‘Generic’?
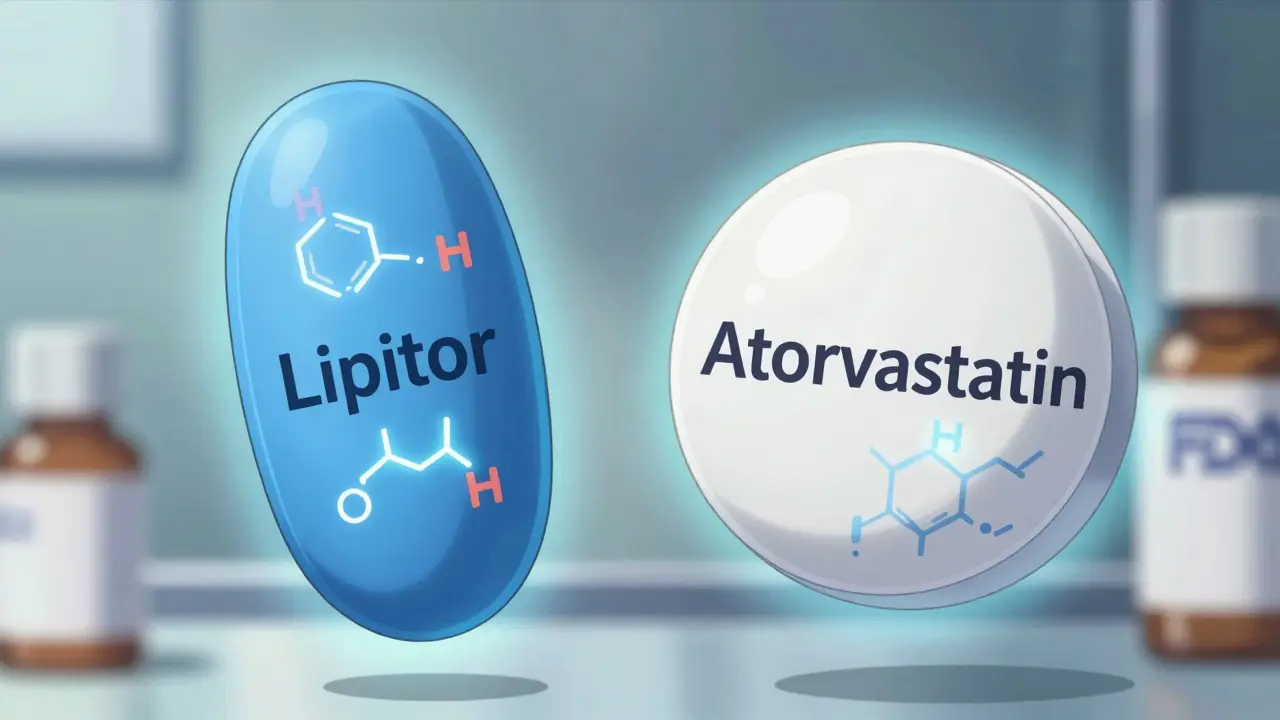
A generic drug isn’t a copy. It’s an exact match in active ingredients. That means the chemical that actually treats your condition - whether it’s high blood pressure, diabetes, or depression - is identical to the one in the brand-name version. The FDA requires this. No exceptions. Every generic must contain the same active ingredient, in the same strength, and delivered the same way - pill, injection, inhaler, you name it. But here’s where people get confused: the pills look different. Maybe the brand is blue and oval. The generic is white and round. That’s not because it’s weaker. It’s because U.S. trademark laws forbid generics from looking exactly like the original. The shape, color, or even the flavoring can change. But none of that affects how the drug works in your body. The real test? Bioequivalence. Before a generic hits the shelf, the FDA makes sure it delivers the same amount of medicine into your bloodstream at the same speed as the brand-name drug. The standard? Between 80% and 125% of the original’s absorption rate. For drugs where tiny changes matter - like blood thinners or thyroid meds - the range tightens to 90% to 111%. That’s not a loophole. That’s precision.Why Are Generics So Much Cheaper?
Brand-name drugs cost a fortune because their makers spent years and hundreds of millions developing them. They ran clinical trials, paid for marketing, and held exclusive rights thanks to patents. Once that patent expires - usually after 12 to 14 years - other companies can step in. Generic manufacturers don’t have to repeat those expensive trials. They just need to prove their version behaves the same in the body. That cuts development costs by 90%. No advertising budgets. No celebrity endorsements. No fancy packaging. So the savings get passed on. The numbers don’t lie. In 2022, generics made up 90% of all prescriptions filled in the U.S. But they accounted for only 25% of total drug spending. Meanwhile, brand-name drugs - just 10% of prescriptions - made up 75% of the bill. That’s $1.67 trillion saved over a decade, according to the Congressional Budget Office. On average, switching to a generic saves you $313 per prescription.When Generics Might Not Be the Best Fit
For most people, generics are a no-brainer. But there are exceptions. Some drugs have what’s called a narrow therapeutic index. That means the difference between a helpful dose and a dangerous one is tiny. Warfarin, levothyroxine, and certain seizure medications fall into this category. Some patients report changes when switching - like feeling more tired, or having seizures return. In rare cases, those reports are real. But studies show it’s usually not the drug itself. It’s the body adjusting to a new inactive ingredient - the fillers, dyes, or binders that hold the pill together. These don’t treat the condition, but they can affect how quickly the medicine dissolves. The FDA has studied this. A 2019 JAMA study of 38,000 patients on levothyroxine found no difference in outcomes between brand and generic. Still, some doctors prefer to keep patients on the same version - brand or generic - to avoid any possible disruption. If you’re on one of these drugs and you switch, watch for changes. Tell your doctor if you feel off.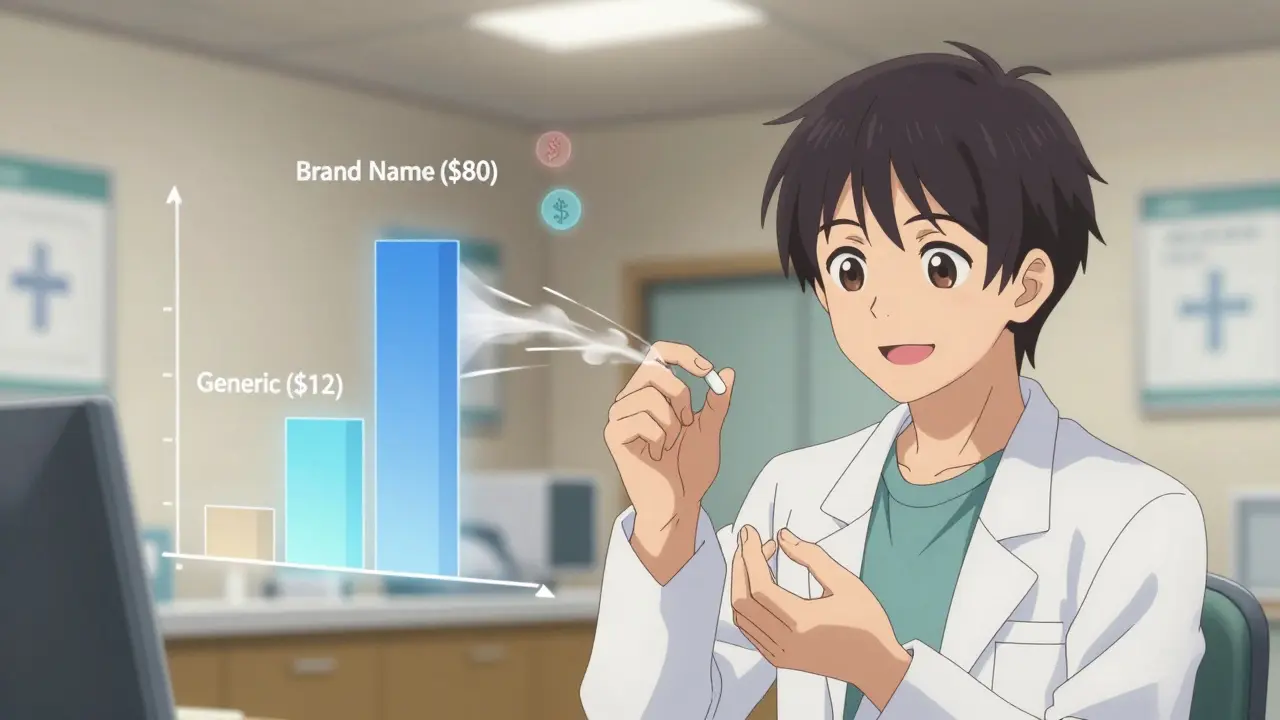
What the Experts Say
The FDA is clear: “All drugs, including brand-name and generic, must work well and are safe.” That’s not marketing speak. It’s a legal requirement. Pharmacists, doctors, and medical associations agree. The American Medical Association says doctors should prescribe generics when appropriate. Pharmacists at Cedars-Sinai confirm generics go through the same rigorous testing and monitoring as brand-name drugs. Even the U.S. government’s own reports back this up. Reddit threads, patient surveys, and pharmacy studies paint the same picture. In one survey of 1,247 people, 89% said generics were just as effective. On r/Pharmacy, over 85% of users reported no difference when switching from brand to generic for common meds like lisinopril, metformin, or atorvastatin. One person saved $400 a month on their asthma inhaler with zero loss of control. But a small group - about 14% - did notice issues. One user said their mom’s seizures returned after switching from Lamictal to generic lamotrigine. She had to go back to the brand. That’s why it’s important to speak up if something feels off. It’s not common. But it happens.How to Use Generics Wisely
In 49 states, pharmacists are required to swap in a generic unless your doctor writes “dispense as written” on the prescription. That’s the law. But you have control too. Keep a simple list: write down the name of every drug you take - both brand and generic. If your prescription changes from “Lipitor” to “atorvastatin,” you’ll know it’s the same thing. Don’t assume the pharmacist will explain it. Ask. If you’re on a high-risk drug - like warfarin, thyroid meds, or epilepsy treatment - stick with one version. If you’ve been on the brand for years, stay on it. If you’ve been on the generic for months with no problems, don’t switch back unless your doctor says so. And always check your bill. Sometimes, the pharmacy will try to charge you more for the brand even when a generic is available. That’s not legal. Ask for the generic price. Use tools like GoodRx to compare costs before you fill the script.

9 Responses
Just switched my blood pressure med to generic last month. No difference at all. Saved $280 this quarter. My pharmacist said the FDA tests these things harder than most people test their coffee maker. Honestly, if it works, why pay more?
Yeah right. The FDA is in bed with Big Pharma. You think they’d let some sketchy factory in India make the same pill as Lipitor? That’s why so many people get weird side effects - the fillers are toxic. I’ve seen the documents. They hide the real ingredients under ‘inactive.’ Don’t be fooled.
My mom’s on levothyroxine and we stuck with the brand after she felt off switching - just to be safe. 😊 But honestly? After 3 years on generic for her cholesterol, zero issues. I get why people worry, but most of the time it’s just anxiety talking. 🤷♀️
For anyone nervous about switching: talk to your pharmacist. They know the ins and outs. And if you’re on something like warfarin or seizure meds, keep the same version - brand or generic - unless your doctor says otherwise. Consistency matters more than you think.
USA think they can fool the world with this generic scam. In Nigeria we know real medicine - not this cheap plastic pills from China. Your body will pay later. Always buy original. Only fools trust FDA. We have real doctors here, not corporate bots.
Generic works fine for metformin. No drama. But if you feel weird after switching it’s probably your mind. Stop blaming the pill. Your anxiety is the active ingredient here
I’m from the Philippines and we use generics all the time. They’re cheaper, yes, but they also save lives. My cousin with diabetes? He couldn’t afford the brand. Generic kept him alive. That’s not a knockoff. That’s justice.
Love that this post breaks it down so clearly. If your doctor prescribes a brand, just ask: ‘Is there a generic?’ Nine times out of ten, yes. And if your pill looks different? Cool. Same medicine. Save your cash for something fun. 🙌
OMG YES!! I switched my atorvastatin to generic last year and my bill dropped from $190 to $12!! I was terrified, but my pharmacist said ‘trust the science’ - and she was right!! No side effects, no weird feelings, just savings!! Everyone should do this!!