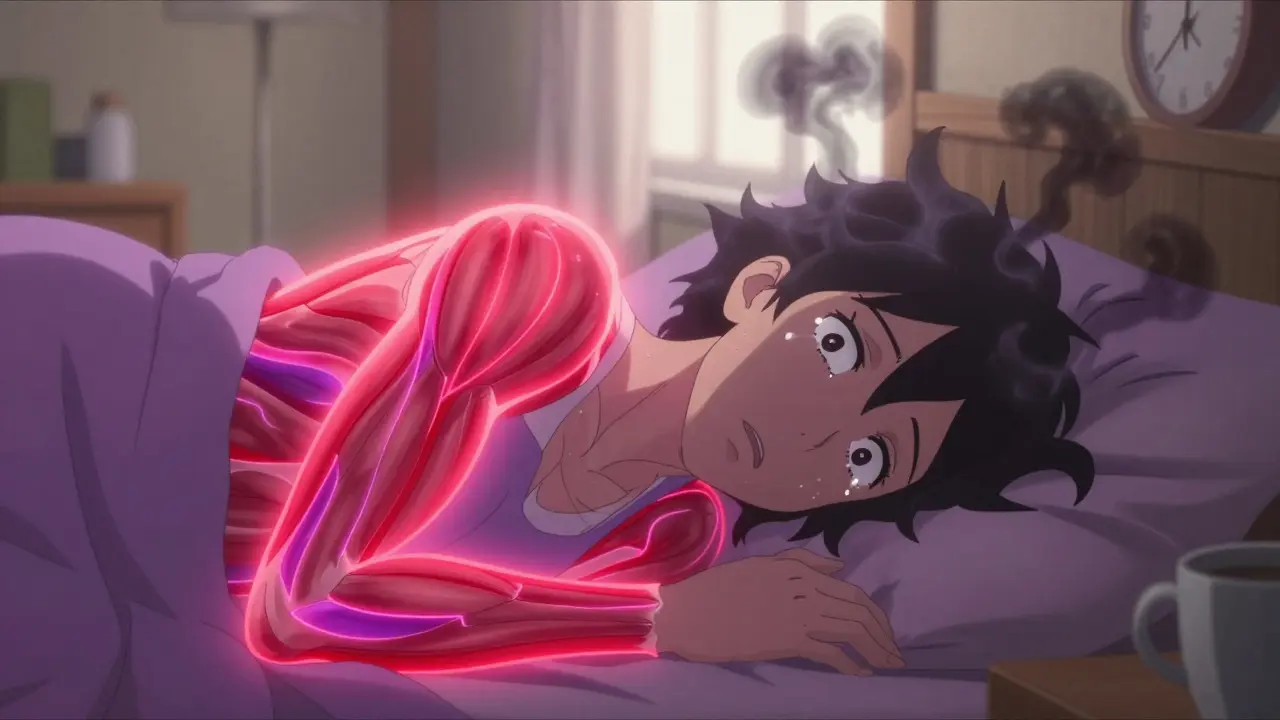
For millions of people, waking up feeling like they’ve been hit by a truck isn’t just a bad day-it’s their normal. Fibromyalgia isn’t just muscle aches. It’s a constant, deep, whole-body pain that doesn’t show up on X-rays or blood tests. Along with it comes crushing fatigue, trouble remembering simple things (called ‘fibro fog’), and sleep that never feels restful. And even though it’s been recognized since 1990, many still think it’s ‘all in your head.’ It’s not. It’s a real neurological condition where the brain and nervous system amplify pain signals. The good news? You don’t have to just live with it. The better news? The most effective treatments aren’t pills-they’re movement, mindfulness, and time.
What Fibromyalgia Really Feels Like
Imagine every muscle in your body aching, like you ran a marathon without ever leaving your bed. Now add a constant buzz of sensitivity-light touches hurt, cold air feels sharp, and even a hug can be overwhelming. That’s the baseline for many with fibromyalgia. The pain isn’t localized. It’s widespread: above and below the waist, on both sides of the body, lasting at least three months. It’s not arthritis. It’s not a pinched nerve. It’s your nervous system stuck on high volume.
Alongside the pain, fatigue hits like a wall. Not just tired-you’re drained, even after 10 hours of sleep. Cognitive fog makes it hard to find words, follow conversations, or remember where you put your keys. Mood swings, anxiety, and depression aren’t just side effects-they’re part of the same neurological storm. The American College of Rheumatology updated its diagnostic criteria in 2016 to reflect this: you don’t need tender points anymore. You need widespread pain plus at least four of these: sleep problems, fatigue, cognitive issues, headaches, irritable bowel symptoms, or numbness.
Why Antidepressants Are Used-Even If You’re Not Depressed
It’s confusing. Why give someone with chronic pain a drug meant for depression? The answer lies in how the brain processes pain. Antidepressants like duloxetine and amitriptyline don’t fix your mood-they tweak the chemicals in your spinal cord and brain that control pain signals. Think of them as volume knobs for pain. They don’t silence it, but they turn it down.
Three antidepressants are FDA-approved specifically for fibromyalgia: duloxetine (Cymbalta), milnacipran (Savella), and pregabalin (Lyrica). Pregabalin isn’t technically an antidepressant-it’s a gabapentinoid-but it’s grouped with them because it works on similar pathways. Then there’s amitriptyline, a tricyclic antidepressant not officially approved for fibromyalgia but prescribed off-label in 60% of cases. It’s cheap, effective for sleep, and often the first choice for older patients.
Here’s what the numbers say: in clinical trials, these medications reduce pain by about 20-30% in about half the people who take them. That sounds low, but for someone in constant pain, even a 25% drop can mean the difference between staying in bed and making it to the grocery store. Duloxetine typically starts at 30mg daily, with increases to 60mg after four weeks. Amitriptyline starts at 5-10mg at bedtime-low enough to avoid next-day grogginess. Most people feel some relief in 4-6 weeks. But here’s the catch: side effects are common. Dry mouth, dizziness, weight gain, nausea, and sleepiness lead 25-30% of patients to quit. One patient on r/fibromyalgia wrote: ‘Duloxetine gave me energy but made me feel like I was being electrocuted inside. I had to stop.’
The Treatment That Actually Works Better Than Pills
Here’s the truth most doctors won’t say loud enough: exercise is the most powerful treatment for fibromyalgia. Not pills. Not injections. Movement. The American College of Rheumatology calls it the single most effective therapy. And yet, it’s the most underused.
Studies show regular, low-impact exercise reduces pain by 25-35% after six months-better than any drug. The trick? Start tiny. Do 10-15 minutes of walking, tai chi, or water aerobics two or three times a week. Don’t push through pain. That’s how flare-ups happen. Instead, use the 10% rule: increase your activity by no more than 10% each week. A 2022 Arthritis Foundation study found yoga reduced pain intensity by 24%. Tai chi improved pain by 20-30% in just 12 weeks. Pilates helped with stiffness and balance. The goal isn’t fitness-it’s rewiring your nervous system to stop seeing movement as a threat.
One woman in Birmingham, who’d been on duloxetine for two years with little relief, started doing seated yoga videos at home. After eight weeks, she cut her pain medication in half. ‘I didn’t feel better because I got stronger,’ she said. ‘I felt better because my body stopped screaming every time I moved.’

How Medications Stack Up Against Other Options
Not all treatments are created equal. Here’s how they compare based on real-world results:
| Treatment | Pain Reduction | Time to Notice Effect | Side Effect Discontinuation Rate | Long-Term Benefit |
|---|---|---|---|---|
| Exercise (walking, tai chi, yoga) | 25-35% | 8-12 weeks | 10-15% | High-sustained for years |
| Duloxetine (SNRI) | 20-30% | 4-6 weeks | 25-30% | Moderate-often fades after 12 months |
| Amitriptyline (TCA) | 25-30% | 2-4 weeks (sleep), 6-8 weeks (pain) | 25-30% | Moderate-best for sleep-focused cases |
| Pregabalin (Lyrica) | 25-40% | 2-4 weeks | 30-35% | Low-dizziness and weight gain limit use |
| Cognitive Behavioral Therapy (CBT) | 20-30% | 8-12 weeks | 5-10% | High-teaches coping skills |
| Acupuncture | 15-25% | 6-12 sessions | 5-10% | Moderate-requires ongoing sessions |
Notice something? The best long-term results come from non-drug treatments. Medications give faster relief, but they often stop working-or become too hard to tolerate. Exercise and CBT don’t just mask pain. They teach your body and brain to respond differently to stress and movement. And they stick.
The Realistic Path Forward: Start Here
If you’ve just been diagnosed, here’s what to do next-no fluff, no hype.
- Get educated. Read the CDC’s free online course ‘Managing Fibromyalgia.’ Know your symptoms. Understand this isn’t weakness-it’s neurology.
- Start moving. Walk for 10 minutes, three times this week. No more. If you feel worse the next day, you went too far. Next week, add one minute. Slow is the new fast.
- Try low-dose amitriptyline. If sleep is your biggest issue, ask your doctor for 5-10mg at bedtime. Don’t start at 25mg. Many people get relief without side effects at this level.
- Find a CBT therapist. Look for one experienced with chronic pain. Twelve weekly sessions can rewire how you react to pain. Insurance rarely covers it-but it’s worth fighting for.
- Hold off on pregabalin or high-dose SNRIs. Save them for if the basics don’t work. Their side effects often outweigh the benefits.
One patient told me: ‘I spent $12,000 on medications that didn’t help. Then I started walking with my dog every morning. Two years later, I’m off all pills. I still have pain-but I’m not controlled by it anymore.’
What’s Changing Right Now
The field is shifting. In 2023, the American College of Rheumatology made it clear: exercise comes first. Medications are second-line. The NIH just funded $15 million to study why the nervous system goes haywire in fibromyalgia. A new drug, centanafadine, showed 35% pain reduction in trials with fewer side effects-and it’s under FDA review. Digital tools like the Quell device, which uses nerve stimulation through the skin, are now FDA-cleared and covered by some insurers.
But the biggest change? Perception. Fibromyalgia is no longer dismissed as ‘psychosomatic.’ It’s recognized as a central nervous system disorder. That means more research, more funding, and more hope.
What to Do When Nothing Seems to Work
It’s okay to feel frustrated. Some people try everything-meds, yoga, acupuncture, diet changes-and still struggle. That doesn’t mean you’re failing. It means you need a different strategy.
Try ‘pacing.’ Instead of doing too much on good days and crashing, spread your activities evenly. Use a notebook to track energy levels. On a 5-point scale, mark how you feel each hour. You’ll start seeing patterns. Maybe you’re fine in the morning but collapse after lunch. Adjust your day around that.
Join a support group. The Fibromyalgia Support Group on Reddit has over 100,000 members. You’ll find people who’ve tried the same drugs, had the same side effects, and found small wins. One person wrote: ‘I can’t run anymore. But I can garden for 15 minutes without crying. That’s my victory today.’
Remember: fibromyalgia isn’t a race. It’s a long walk with ups and downs. The goal isn’t to be pain-free. It’s to live well despite the pain.
Can antidepressants cure fibromyalgia?
No. There is no cure for fibromyalgia. Antidepressants help manage symptoms by reducing pain signals in the brain and improving sleep, but they don’t fix the underlying neurological sensitivity. They’re tools for symptom control, not a solution.
Why do doctors prescribe antidepressants if I’m not depressed?
They’re prescribed because these drugs affect neurotransmitters like serotonin and norepinephrine, which regulate pain signals in the spinal cord and brain-not mood. Research shows they reduce pain intensity even in patients with no history of depression. It’s about neurology, not psychology.
How long does it take for antidepressants to work for fibromyalgia pain?
It varies. Amitriptyline often helps with sleep in 2-4 weeks, but pain relief may take 6-8 weeks. SNRIs like duloxetine usually show pain reduction in 4-6 weeks. Don’t stop if you don’t feel better right away. Give it time-and talk to your doctor about side effects.
Are there natural alternatives to antidepressants for fibromyalgia?
Yes. Exercise (especially tai chi and yoga), cognitive behavioral therapy (CBT), acupuncture, and mindfulness practices have strong evidence for reducing pain and improving function. These are often more effective long-term than medications and come with fewer side effects. Many people combine them with low-dose meds for better results.
What’s the most important thing to do if I have fibromyalgia?
Start moving-gently and consistently. Exercise is the single most effective treatment, proven to reduce pain more than any medication over time. Don’t wait until you feel better to start. Start small, stay steady, and let your body adapt. Movement reprograms your nervous system. That’s the foundation of long-term relief.
Final Thought: It’s Not About Fighting Pain-It’s About Living Around It
You don’t need to be cured to live well. Fibromyalgia doesn’t have to be the boss of your life. The most successful people aren’t the ones who eliminate pain. They’re the ones who learned how to move through it-with patience, strategy, and a little bit of stubborn hope.

13 Responses
Just wanted to say this post hit different. I’ve been living with fibro for 7 years, and the part about movement reprogramming the nervous system? That’s the exact thing my PT told me-but I didn’t believe it until I tried 10-minute water aerobics. No magic pills. Just consistency. Now I can carry groceries without crying. Small wins matter.
Let’s be real-most people who preach ‘exercise is the cure’ have never had a flare-up so bad they couldn’t lift their own head. This isn’t laziness. It’s neurology. And yes, antidepressants work for some of us. Don’t dismiss meds because you got lucky.
Agreed. The 10% rule is everything. Push too hard, and you set yourself back weeks. Slow progress is real progress. I started with 5 minutes of stretching. Now I walk 2 miles daily. No drugs. Just patience.
It’s not just the nervous system-it’s the somatic memory of trauma, the epigenetic imprint of chronic stress, the limbic system’s betrayal of the body’s innate wisdom. We’re not treating pain-we’re negotiating with a wounded autonomic nervous system that learned to scream to survive. Antidepressants? They’re temporary bandages on a systemic wound. Movement? That’s the slow, sacred act of re-remembering safety.
Man, I love how you said ‘live around it’-that’s my mantra now. I still have pain, but I cook dinner, play with my niece, and even hike short trails. I use Quell now. It’s not perfect, but it’s a game-changer. And yeah, I cried the first time I walked my dog without needing to sit down after 3 minutes. 💪
There’s a deeper layer here: fibro isn’t just a disease-it’s a cultural mirror. We live in a world that equates productivity with worth. So when your body says ‘no,’ society says ‘you’re broken.’ That’s why CBT works-it’s not about changing your thoughts, it’s about reclaiming your right to rest. The real cure? A society that stops punishing people for being human.
Anyone who says exercise is ‘better than pills’ is ignoring the fact that many of us can’t move without triggering a 3-day crash. Your privilege is showing. I’ve tried yoga, walking, tai chi-I spent 6 months trying to ‘earn’ relief. I ended up in the ER. Don’t preach. Listen.
I hear you. I’m one of those who tried everything and crashed harder. What changed? I stopped trying to ‘beat’ fibro and started negotiating with it. I schedule rest like meetings. I say no without guilt. And I take 10mg of amitriptyline-just enough to sleep. Not perfect. But I’m alive. And that’s enough.
Oh, the noble ‘movement is medicine’ crusade-how quaint. Like yoga and kombucha are the new holy trinity of chronic illness. Meanwhile, real people are on disability, crying in their cars because they can’t button their shirts. Let’s stop romanticizing suffering and acknowledge that for many, meds are the only thing keeping them from total collapse.
As someone from India where fibromyalgia is rarely diagnosed, I’ve spent years being told it’s ‘stress’ or ‘weak nerves.’ This article is the first thing that felt like truth. I started walking after sunset-no one sees me struggle. I take amitriptyline at 5mg. I sleep better. I don’t feel like a fraud anymore. Thank you for writing this.
Just a quick note: I’ve been on Lyrica for 3 years. It helped my pain by 30%, but the brain fog and weight gain were brutal. I tapered off last year. Started CBT + daily seated stretches. Now I’m at 20% pain, no meds. Not ‘cured’-but I’m functional. And that’s the goal, right?
The NIH funding $15M? That’s huge. It means they’re finally taking this seriously. I’ve been waiting 12 years for someone to say: ‘This isn’t in your head.’ We’re not broken. We’re misunderstood. And now, science is catching up.
One sentence: I stopped chasing ‘cure’ and started chasing ‘better days.’ Now I have more of them.