By 2026, more than 1 in 5 commonly prescribed medications in the UK and US could be unavailable for weeks or months at a time. This isn’t speculation-it’s what experts are seeing in supply chain data, manufacturing reports, and hospital inventory logs. The problem isn’t just about one factory shutting down or a raw material delay. It’s about a system under pressure from climate shocks, geopolitical splits, aging populations, and shrinking profit margins for generic drugs. If you’re taking blood pressure pills, antibiotics, insulin, or even something as basic as ibuprofen, you’re already in the crosshairs of a growing crisis.
Why Drug Shortages Are Getting Worse
Drug shortages used to be rare events. A single plant failure, a hurricane, or a regulatory inspection could knock out a medicine for a few months. Now, they’re systemic. The World Health Organization estimates that 1 in 4 essential medicines globally face supply disruptions at least once a year. In the UK, the NHS reported 412 active drug shortages in mid-2025-up from 287 in 2022. Why the jump?
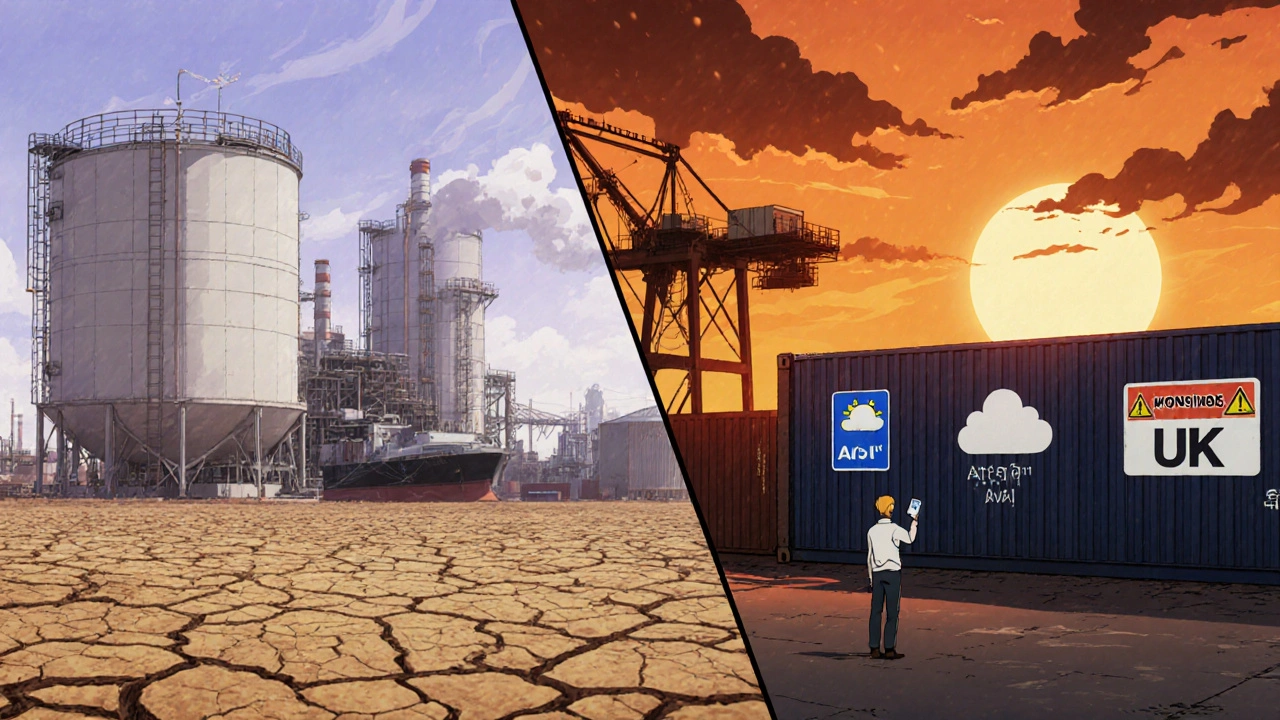
It starts with where drugs are made. Over 80% of active pharmaceutical ingredients (APIs) for medicines sold in the UK and US come from just two countries: China and India. Both face growing internal pressures. In China, environmental crackdowns have shut down dozens of API factories since 2023. In India, water shortages in the Hyderabad region-where nearly half the world’s generic drug ingredients are produced-have forced production cuts. The same water stress that’s hurting crops is now hurting your pills.
Then there’s the economics. Generic drugs are cheap. Very cheap. A 30-day supply of metformin might cost £2.50 in the UK. Manufacturers barely make a profit. So when costs rise-due to energy prices, shipping delays, or new regulations-they walk away. They don’t invest in backup lines or extra inventory. They just stop making it. And when one company stops, others don’t step in fast enough. The market doesn’t reward preparedness. It rewards lowest price.
How Forecasting Works Now
Forecasting drug shortages today isn’t guesswork. It’s data-driven systems analysis. Agencies like the UK’s MHRA and the US FDA now track over 200 signals: factory inspections, raw material shipments, export bans, patent expirations, even weather patterns in manufacturing regions. The most accurate models combine these with economic indicators-like the cost of solvents, electricity prices in Gujarat, or shipping rates from Shanghai to Liverpool.
For example, in early 2025, a spike in ammonia prices in China triggered a red flag. Ammonia is a key ingredient in making antibiotics like amoxicillin. Within six weeks, the FDA issued a warning: amoxicillin supplies could drop by 40% by Q3. Hospitals started rationing. Pharmacies switched to alternatives. That’s forecasting in action-not predicting the future, but spotting the warning signs before the crisis hits.
These systems also look at demographic shifts. The UK’s population over 65 will grow by 22% by 2030. Older people take 5-7 medications on average. More seniors = more demand for heart meds, diabetes drugs, painkillers. But production hasn’t scaled. The supply chain is built for 2015, not 2030.
Climate and Geopolitics Are the Wild Cards
Climate change isn’t just about floods and fires. It’s about factory closures, transport delays, and ingredient shortages. In 2024, monsoon floods in India disrupted the supply of citric acid-a key stabilizer in injectable drugs. Production halted for 11 weeks. That one event caused shortages of 17 different medications across Europe.
Geopolitics is even more unpredictable. The war in Ukraine disrupted the supply of neon gas, used in manufacturing semiconductors for infusion pumps. The Red Sea shipping crisis pushed delivery times for pharmaceuticals from Asia to Europe from 21 days to 45. The US-China trade tensions led to new export controls on rare earth elements used in drug packaging machinery. Each of these events was small on its own. Together, they created a ripple effect that no single company could absorb.
And then there’s the new reality: dual sourcing is no longer optional. In 2025, 63% of major pharmaceutical companies started building backup manufacturing sites outside China and India. Some moved to Poland, others to Mexico. But setting up a new API plant takes 3-5 years and £200 million. It’s not something you do overnight.
Who’s Most at Risk?
It’s not just patients. It’s hospitals, GPs, and pharmacists too. But some groups feel the pinch harder.
- Chronic disease patients: Those on long-term meds like warfarin, levothyroxine, or insulin face dangerous gaps. Switching brands can mean dosage changes, side effects, or hospital visits.
- Cancer patients: Chemotherapy drugs like doxorubicin and vincristine have no alternatives. Shortages here can delay life-saving treatment.
- Children: Paediatric formulations are made in tiny batches. When a factory shuts down, there’s no spare stock. Kids go without.
- Low-income households: If your medicine isn’t on the NHS list, and the alternative costs £80 instead of £2, you skip doses.
And it’s not just about availability-it’s about quality. When demand spikes and supply is tight, some manufacturers cut corners. In 2024, the MHRA recalled 12 batches of generic metformin after detecting trace carcinogens. That wasn’t a manufacturing error. It was a cost-cutting one.
What’s Being Done-and What’s Not
The UK government launched the Pharmaceutical Supply Chain Resilience Strategy in early 2025. It includes:
- Stockpiling 6 months’ supply of 50 critical medicines (mostly antibiotics, anaesthetics, and insulin)
- Subsidising UK-based API production with £120 million in grants
- Requiring manufacturers to report inventory levels monthly
But here’s the catch: stockpiles only help if you know what’s coming. Forecasting tools still miss 30-40% of shortages because they can’t predict sudden political moves or climate events. And subsidies don’t fix the core problem: generic drugs aren’t profitable.
Some companies are trying new models. A few UK pharmacies now offer subscription services for high-risk meds-buying in bulk, storing safely, and delivering directly to patients. Others are partnering with universities to build local API labs. But these are pilot projects. Not policy.

What You Can Do Right Now
If you’re on a long-term prescription, don’t wait for a shortage to hit.
- Ask your GP or pharmacist: Is your drug made in China or India? Are there alternatives? Not all generics are the same-some have better supply chains.
- Keep a 14-day buffer: If your prescription allows, ask for a 90-day supply. Many pharmacies can help with this.
- Sign up for alerts: The NHS and MHRA send out shortage warnings via email. Register at www.nhs.uk/medicines-alerts.
- Don’t stockpile: Hoarding creates artificial shortages. Trust the system, but prepare.
And if you’re a healthcare worker: push for transparency. Demand that your hospital tracks drug inventory in real time. Use the NHS’s new Supply Chain Dashboard-it’s free, and it shows live shortage levels for over 300 drugs.
The Bottom Line
Drug shortages aren’t going away. They’re becoming the new normal. But they don’t have to be a crisis. With better forecasting, smarter policy, and a shift away from ultra-cheap generics, we can build a system that doesn’t break under pressure. The data is there. The tools exist. What’s missing is the will to invest in prevention-instead of just reacting to the next emergency.
By 2030, the number of drugs at risk of shortage could double. The question isn’t whether it will happen. It’s whether we’re ready to stop treating it as a surprise-and start treating it as a design flaw.
Why are generic drugs more likely to have shortages than brand-name ones?
Generic drugs are made by multiple manufacturers who compete on price, not quality or reliability. Since profit margins are razor-thin-sometimes under 5%-companies stop making them when costs rise or demand dips. Brand-name drugs, by contrast, have patent protection and higher prices, so manufacturers invest in backup production lines, inventory, and quality control. There’s simply no financial incentive to prepare for shortages with generics.
Can the UK produce its own medicines to avoid shortages?
Yes, but it’s slow and expensive. The UK has the technical ability to make APIs and finished drugs, but it stopped doing so decades ago because it was cheaper to import. Rebuilding domestic capacity requires billions in investment, new regulations, and trained workers. The government’s £120 million grant is a start, but it’s less than 10% of what’s needed to replace even 20% of current imports. Local production won’t solve everything, but it can reduce risk for critical drugs like insulin or adrenaline.
Are drug shortages getting worse because of Brexit?
Brexit added complexity, but it didn’t cause the problem. Before Brexit, the UK relied on EU-wide supply chains. Now, medicines crossing borders face extra paperwork, inspections, and delays. That makes small disruptions bigger. But the root causes-China/India dependency, low generic profits, climate stress-are global. Brexit made the UK more vulnerable, but the system was already fragile.
How far ahead can drug shortages be predicted?
Most shortages are predicted 3-6 months in advance using supply chain data. Some models, like those used by the FDA and MHRA, can flag risks up to 12 months ahead if there’s a clear trend-like a factory closure notice or a sudden spike in raw material prices. But sudden events (natural disasters, political bans, cyberattacks) can still catch systems off guard. The best forecasts combine data with expert judgment, not just algorithms.
What should I do if my medicine is on shortage list?
Don’t stop taking it. Contact your GP or pharmacist immediately. They can check for alternatives, switch you to a different brand, or order from a supplier with stock. Some pharmacies have access to emergency stocks or can source from EU suppliers. Never substitute without professional advice-especially for drugs like warfarin, thyroid meds, or epilepsy treatments. Even small differences in formulation can be dangerous.


13 Responses
This is wild but also... kinda predictable? Like we knew this was coming when we outsourced everything to save a few bucks. 😅 Time to start treating medicine like infrastructure, not a commodity.
The data on API production shifts is solid. I’ve seen the shipment logs from Gujarat-water shortages are forcing 30% capacity cuts. What’s not being discussed is how much of this is tied to groundwater depletion, not just climate. This is a resource crisis disguised as a supply chain issue.
Let’s be real-this is what happens when you let China and India run the world’s medicine cabinet. We’re one trade war away from a national health emergency. Time to bring manufacturing home or start rationing meds like during WWII.
generic drugs are cheap because theyre garbage anyway. who needs metformin when you can just eat less sugar? lol. also why are we even talking about this like its a surprise? we knew this was gonna blow up. #capitalism
The NHS stockpile? A distraction. The real agenda is consolidation-big pharma buying up smaller suppliers, creating artificial scarcity to justify price hikes. The government’s 'resilience strategy' is just a PR stunt to keep the public from asking who profits when people can’t get insulin.
India producing 40% of global generics? That’s cute. But did you know most of those 'Indian-made' APIs are actually Chinese intermediates shipped through Gujarat? The whole supply chain is a house of cards built on labor exploitation and environmental neglect. We’re all complicit.
We treat medicine like toilet paper-buy it cheap, use it fast, throw it away. But when the toilet paper runs out, you don’t just cry-you learn to make your own. Maybe it’s time we stop outsourcing our survival to corporations who don’t care if we live or die.
This is not just about drugs. It's about how we value life in a system that measures everything in quarterly returns. We built a world where profit is the only language that matters. Now the language is failing us. We need to learn a new one.
The forecasting models are robust but limited by input fidelity. The real bottleneck is data latency-many factories still report via fax. If we integrated IoT sensors on API storage units and fed that into ML pipelines, we could reduce false negatives by 60%. This isn't sci-fi-it's operational logistics.
If you’re on a long-term med, talk to your pharmacist. Seriously. They know which batches are from Poland vs. Shanghai. And if you can get a 90-day script, do it. Small steps save lives. You’re not hoarding-you’re being smart.
I’m from Ireland and we’ve been hit hard by Red Sea delays. My mum’s blood thinner was out for 6 weeks. The pharmacy called me crying. We need global solidarity here-not blame games. 🙏 Let’s fund local production where we can, but also support the workers in India and China who make this possible.
The real tragedy? We have the tech. We have the data. We have the money. What we don’t have is the moral imagination to treat healthcare like a human right instead of a market segment. We’re not facing a shortage of drugs. We’re facing a shortage of decency.
The assertion that generic drugs are inherently less reliable is misleading. Quality control standards are enforced by the MHRA and FDA regardless of origin. The issue is not quality-it is economic disincentive. Manufacturers are rational actors responding to market signals. The solution is not nationalism but structural economic reform.