When your immune system turns against your own body, things get messy fast. Autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis don’t just cause discomfort-they can damage organs, cripple mobility, and steal years of your life. That’s where corticosteroids come in. These aren’t the bodybuilding steroids you hear about in sports news. These are powerful, lab-made versions of cortisol, the hormone your adrenal glands make naturally to manage stress and inflammation. For decades, they’ve been the go-to tool to slam the brakes on runaway immune attacks. But here’s the catch: they work too well. And that’s where the real trouble starts.
How Corticosteroids Stop Autoimmune Damage
Corticosteroids like prednisone and methylprednisolone don’t just mask symptoms-they shut down the fire at its source. Inside your cells, they bind to receptors that control gene activity. This turns off the production of inflammatory proteins like TNF-alpha, interleukins, and enzymes that tear through tissue. They also reduce the number of white blood cells and macrophages rushing to the site of damage. The result? Swelling drops, pain fades, and organ function improves-sometimes within hours.
That speed is why doctors reach for corticosteroids first. If you’re diagnosed with rapidly progressive glomerulonephritis or severe lupus nephritis, waiting weeks for methotrexate or azathioprine to kick in isn’t an option. Corticosteroids act fast. In acute cases like Guillain-Barré syndrome or severe asthma flare-ups, a high-dose IV pulse of methylprednisolone can mean the difference between hospitalization and walking out the door.
For many, it’s life-changing. A patient with polymyalgia rheumatica might wake up one day unable to lift their arms. After a few days on low-dose prednisone, they’re back to brushing their hair. That’s not magic-it’s targeted suppression of inflammation at the molecular level.
When Corticosteroids Don’t Work
But they’re not a cure-all. In advanced type 1 diabetes, where insulin-producing beta cells are already destroyed, corticosteroids won’t bring them back. The same goes for Hashimoto’s thyroiditis in its late stages, Graves’ disease, or advanced primary biliary cholangitis. These aren’t inflammatory flare-ups-they’re end-stage organ failure from long-term immune destruction. Steroids can’t rebuild what’s gone.
Even in diseases where they help, like multiple sclerosis, the effect is temporary. They reduce relapse severity but don’t stop nerve damage from accumulating over time. That’s why newer drugs like ocrelizumab or natalizumab are now preferred for long-term control. Corticosteroids are the emergency siren, not the steady patrol car.
The Hidden Cost: Long-Term Side Effects
Take corticosteroids for more than a few weeks, and the body starts paying the price. The most common problem? Bone loss. Up to 40% of people on long-term prednisone develop osteoporosis. That’s not just a buzzword-it means brittle bones that fracture from a stumble or even a cough. Doctors now routinely prescribe calcium, vitamin D, and bisphosphonates alongside steroids to protect bones, but prevention isn’t always enough.
Cataracts are another silent thief. Clouding of the lens can creep in after months of use, slowly stealing your vision. Many patients don’t notice until their reading glasses no longer help. Regular eye checks become mandatory.
Then there’s weight gain-not the kind from eating too much pizza, but from fat shifting to your face, neck, and belly. Moon face. Buffalo hump. These aren’t myths-they’re real, visible changes caused by altered fat metabolism. Blood sugar spikes are common too. People without diabetes can develop steroid-induced diabetes, requiring insulin or oral meds.
And your immune system? It stays turned down. That means you’re more vulnerable to infections. A simple cold can turn into pneumonia. A cut that normally heals in days might become an abscess. Skin thins out, bruising easily. Some patients develop stretch marks that look like scars. Sun sensitivity increases, making outdoor time risky without strong sunscreen.

Adrenal Insufficiency: The Body Forgets How to Help Itself
One of the most dangerous long-term effects is adrenal suppression. Your body stops making its own cortisol because the pills are doing the job. If you suddenly stop taking steroids, your body can’t ramp up production fast enough. That’s an adrenal crisis-low blood pressure, vomiting, confusion, even death. It’s rare, but it happens.
The good news? If you’ve been on less than 10 mg of prednisone daily for under three weeks, your adrenal glands usually bounce back on their own. But if you’ve been on higher doses for months or years, you need to taper slowly-over weeks or even months. Jumping off cold turkey isn’t just uncomfortable; it’s dangerous.
Doctors check for this by measuring morning cortisol levels after skipping a dose. If your levels are too low, you’re not ready to stop. This isn’t just theory-it’s standard practice in rheumatology clinics across the UK and US.
How to Use Them Safely
Modern treatment doesn’t mean taking high-dose steroids for years. The goal now is to use them as a bridge-not a lifetime anchor. Doctors aim for the lowest dose that controls symptoms. For many, that’s 5 mg or less of prednisone per day, often taken every other day to reduce side effects.
Combination therapy is the new standard. Instead of relying on steroids alone, they’re paired with drugs like methotrexate, azathioprine, or rituximab. These drugs take longer to work but are safer long-term. Once they kick in, the steroid dose gets lowered. In autoimmune hemolytic anemia, adding rituximab to prednisone cuts relapse rates by half.
Topical versions help too. Inhaled steroids for asthma or nasal sprays for allergic rhinitis deliver the drug exactly where it’s needed, with almost no systemic side effects. Same with creams for eczema or psoriasis. The trick is avoiding oral steroids unless absolutely necessary.
What Comes After Steroids?
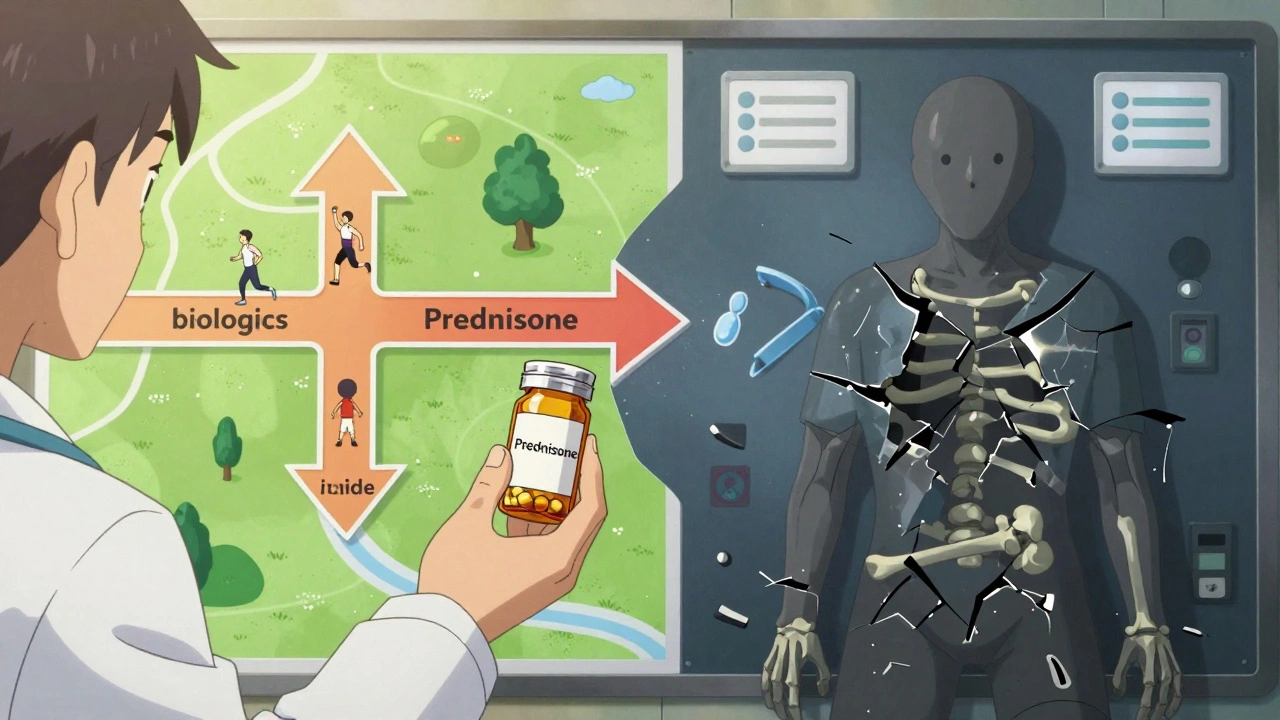
The future isn’t more steroids-it’s smarter alternatives. Biologics like rituximab, belimumab, and tocilizumab target specific immune cells without wiping out the whole system. They’re expensive, yes, but they’re safer for long-term use. In lupus, belimumab reduces flare frequency without the bone loss or diabetes risk of steroids.
Even newer drugs are emerging. Researchers are exploring GILZ-based therapies-proteins that mimic corticosteroids’ anti-inflammatory effects without the side effects. Early trials show promise in rare autoimmune diseases where steroids have been the only option.
The message is clear: corticosteroids are powerful, but they’re not the endgame. They’re the first responder. Your long-term plan should be about getting off them, not staying on them.
What You Should Do If You’re on Steroids
- Take them exactly as prescribed. Never skip or double up without talking to your doctor.
- Get bone density scans yearly if you’ve been on them longer than 3 months.
- See an eye doctor every 6-12 months for cataract checks.
- Monitor your blood sugar. Even if you’ve never had diabetes, steroids can trigger it.
- Always carry a medical alert card or bracelet saying you’re on steroids. In an emergency, this could save your life.
- Never stop abruptly. Tapering must be planned with your doctor.
- Use sunscreen daily. Your skin is more vulnerable to sun damage.
It’s not about fear-it’s about awareness. Corticosteroids are one of the most effective tools we have against autoimmune disease. But they’re a double-edged sword. Used right, they give you back your life. Used wrong, they steal from it.
Can corticosteroids cure autoimmune diseases?
No. Corticosteroids suppress inflammation and calm the immune system, but they don’t fix the underlying cause of autoimmune diseases. They help manage symptoms and prevent damage, but they don’t cure conditions like lupus, rheumatoid arthritis, or multiple sclerosis. Long-term control requires other medications that target specific immune pathways.
How long can you safely take prednisone?
There’s no fixed limit, but the goal is always to use the lowest effective dose for the shortest time possible. Short courses (under 3 weeks) carry minimal risk of adrenal suppression. Long-term use (more than 3 months) increases the risk of osteoporosis, cataracts, diabetes, and infections. Many patients transition to other drugs within 6-12 months to reduce steroid exposure.
Are there natural alternatives to corticosteroids?
No natural remedy can match the potency of corticosteroids for controlling severe autoimmune inflammation. Some supplements like omega-3s or curcumin have mild anti-inflammatory effects, but they’re not replacements. Relying on them instead of prescribed treatment can lead to irreversible organ damage. Always discuss alternatives with your doctor-never stop steroids on your own.
Why do corticosteroids cause weight gain?
Corticosteroids change how your body stores fat and uses sugar. They increase appetite and cause fat to accumulate in the face, neck, and abdomen. They also reduce muscle mass and cause fluid retention. This isn’t just "eating too much"-it’s a direct metabolic effect of the drug. Managing diet and exercise helps, but the change is often unavoidable with long-term use.
What should I do if I miss a dose of corticosteroids?
If you miss a dose, take it as soon as you remember-unless it’s close to your next scheduled dose. Never double up. If you’re on a daily dose and miss more than one day, contact your doctor. Missing doses can trigger withdrawal symptoms or a flare-up. If you’re on a tapering schedule, missing a dose can throw off the whole plan.
Do corticosteroids affect mental health?
Yes. Mood swings, anxiety, insomnia, and even depression or psychosis can occur, especially at higher doses. These effects are more common in people with a history of mental health conditions. If you notice changes in your mood, sleep, or thoughts, tell your doctor. Adjusting the dose or adding support can help.
Final Thoughts
Corticosteroids are a medical miracle-when used wisely. They’ve given millions of people back their ability to walk, breathe, and live without constant pain. But they’re not a long-term solution. The real win isn’t just controlling inflammation-it’s getting off steroids safely. That’s why modern treatment focuses on combining them with safer drugs, monitoring side effects closely, and always having an exit plan. If you’re on them, don’t be afraid to ask: "What’s my path off this?" Your future self will thank you.


13 Responses
This is why I stopped taking prednisone after 6 months. My face looked like a balloon and I started crying for no reason. Like, I literally cried during a dog commercial. 🤮
It’s fascinating how we’ve weaponized a natural hormone to suppress the body’s own defense system. Corticosteroids are a paradox-they save lives by silencing the immune system, yet in doing so, they unravel the very architecture of biological balance. We’re playing god with cortisol, and the bill always comes due.
Maybe the real question isn’t how to use them better, but whether we’re treating the symptom because we’re afraid to confront the root: why did the immune system turn on itself in the first place? Is it toxins? Trauma? The microbiome? We fix the leak but never check the pipe.
And yet… I’d take the moon face over a failing kidney any day. There’s no moral high ground here, only painful trade-offs.
Oh my god, I just got diagnosed with giant cell arteritis last month. They hit me with 60mg of prednisone like it was coffee. I swear, within 48 hours I could lift my arm again. But now? I’m on 10mg and I’ve gained 22 pounds, my skin’s paper-thin, and I had a stress fracture from sneezing.
I’m terrified to taper. My doctor says I’ll be on this for a year minimum. I just want to feel like me again. Not this puffy, anxious, sugar-craving ghost.
Also-why does everyone say ‘just lose the weight’ like it’s a diet problem? I’m eating kale and running 5Ks. My body is literally betraying me. 😭
Important clarification: steroid-induced osteoporosis isn’t just about bone density-it’s about microarchitectural degradation. Even if your DEXA scan looks ‘okay,’ the trabecular connectivity is compromised, making fractures more likely under low-impact stress.
That’s why we combine bisphosphonates with vitamin D3 (1000–2000 IU/day) and calcium citrate (1200 mg/day), not carbonate-absorption is better in low gastric pH, which steroids suppress.
Also, monitor serum 25-OH vitamin D levels every 6 months. Many patients are deficient despite supplementation because steroids accelerate hepatic catabolism. And yes-weight-bearing exercise is non-negotiable. Walking isn’t enough. Do squats. Use resistance bands. Your bones need mechanical load to remodel.
And for the love of science, stop Googling ‘natural steroid alternatives.’ Turmeric doesn’t inhibit NF-kB at clinically relevant concentrations. Don’t risk blindness or renal failure because of a YouTube influencer.
I’ve been on low-dose prednisone for 8 years now. I’m 42. I’ve had two hip replacements. I’ve had cataract surgery on both eyes. I developed type 2 diabetes at 38. I’ve had pneumonia twice because my immune system was too quiet.
And yet-I can still hug my kids. I can still work. I can still cook dinner.
I don’t know if I’d do it again. But I don’t know what else would have kept me alive.
There’s no victory here. Just survival. And a lot of quiet grief.
Everyone here is acting like corticosteroids are some kind of evil drug but let me tell you something from India where we don’t have access to biologics or rituximab. Prednisone is literally the only thing keeping my aunt alive with pemphigus vulgaris. She’s been on 5mg daily for 12 years. She has moon face, osteoporosis, and diabetes but she’s alive and she’s watching her grandchildren grow up. You think you have it bad? Try living in a country where the cheapest biologic costs 10x your monthly salary. Steroids are not the enemy-poverty and lack of healthcare are. Stop being so privileged with your complaints. We don’t get to choose between side effects and death. We choose death less often.
Also, natural alternatives? Bro, I’ve seen people try neem, ashwagandha, and turmeric paste on their open wounds because they couldn’t afford steroids. One woman lost her leg to sepsis. Don’t be that person. Take your pills. And thank your lucky stars you have a doctor who knows what they’re doing.
So… are you saying the government is using steroids in the water to make people docile? Because I’ve noticed my neighbors are all super passive now. And why do all the doctors sound like they’re reading from a pharma pamphlet? I smell a cover-up. Also, my cat got fat after I started taking prednisone. Coincidence? I think not.
Ugh, I can’t believe people still believe this ‘steroids are a bridge’ nonsense. I’ve been on 7.5mg for 11 years and my rheumatologist says ‘we’re just waiting for the next miracle drug.’ But the next miracle drug is always 5 years away and costs $50,000 a year. Meanwhile, I’m on 6 meds just to counteract the side effects. I’m not a patient-I’m a pharmacological experiment. And you all act like this is normal. It’s not. It’s a slow, quiet torture. And the system doesn’t care because you’re not dying fast enough to make headlines.
Also, I’ve been told ‘just exercise’ 47 times. I can’t. My knees are gone. My spine is crumbling. I can’t lift my arms. What am I supposed to do? Yoga with a walker? Please.
omg i was on prednisone for lupus and i thought i was gonna die from the weight gain but then i started drinking lemon water and doing yoga and i lost 30lbs!! now im 100% off steroids and my skin is glowing!! god is good!! 🙏✨
Respectfully, the clinical guidelines from the American College of Rheumatology and the British Society for Rheumatology clearly state that corticosteroid therapy must be individualized with regular monitoring of bone density, glucose tolerance, intraocular pressure, and adrenal axis function. The use of steroid-sparing agents such as methotrexate and mycophenolate mofetil reduces cumulative steroid exposure by up to 60% over three years. Adherence to tapering protocols reduces adrenal crisis risk by 92%. The data is unequivocal. The responsibility lies with the patient to follow medical advice and with the physician to provide clear, structured care. There are no shortcuts in chronic disease management.
yo i just wanna say i was on 20mg for 3 years and i thought i was gonna lose my mind but then i found this therapist who specialized in chronic illness and she helped me reframe it. like, yeah the moon face sucks but i’m alive. yeah i got diabetes but i’m learning to cook. yeah my skin bruises easy but i got my dog back. i used to hate my body but now i see it as this tough-ass warrior that kept me going when everything else wanted to quit. you guys are not alone. we’re all just trying to survive this mess. and hey, if you need to vent, i got u. DM me. we in this together 💪❤️
Look, I don’t care what your doctor says. If you’re on steroids long-term, you’re weak. America doesn’t need pills to fight disease. We need grit. My grandpa fought in Korea with nothing but penicillin and a prayer. You think he took prednisone? No. He suffered. He endured. That’s what made him strong. You people are soft. Take your meds and stop whining. We don’t need more coddling. We need more toughness.
They never tell you the real side effect: the loneliness. You look different. You smell different. You can’t hug people without worrying you’ll bruise them. You’re tired all the time. You can’t sleep. You cry for no reason. You’re told to be grateful you’re alive-but no one asks how you’re living.
It’s not the moon face. It’s the silence.