What Is Coronary Artery Disease?
Coronary artery disease (CAD) happens when the arteries that feed your heart muscle start to narrow. It’s not a sudden event-it builds up over years, often without warning. The main culprit is atherosclerosis, a process where fatty deposits, cholesterol, and other substances stick to the inner walls of your coronary arteries. Over time, these buildups, called plaques, harden and restrict blood flow. When your heart doesn’t get enough oxygen-rich blood, you might feel chest pain, shortness of breath, or even have a heart attack.
What makes CAD dangerous is that it doesn’t always show symptoms until it’s advanced. Many people don’t know they have it until they’re in the emergency room. According to the World Health Organization, ischemic heart disease-mostly caused by CAD-was responsible for 13% of all deaths worldwide between 2000 and 2021. In the U.S. alone, about 18.2 million adults over 20 live with this condition.
How Atherosclerosis Works
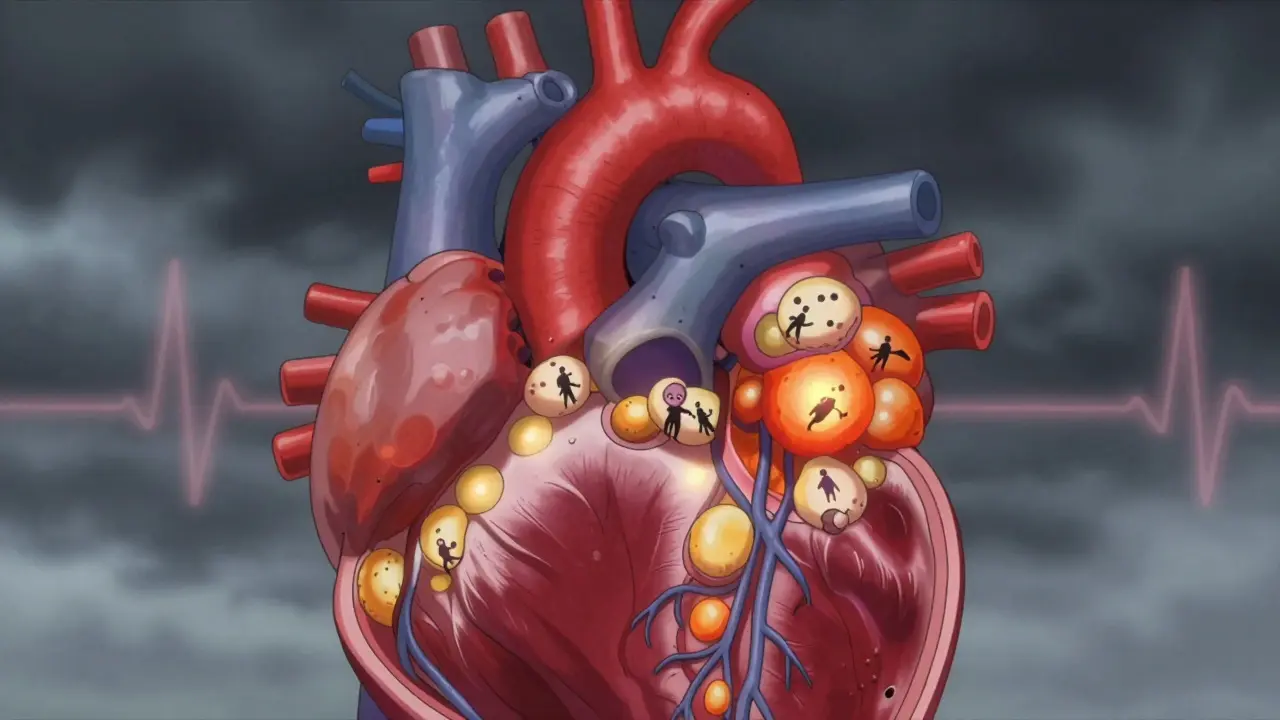
Atherosclerosis isn’t just "clogged pipes." It’s a complex, active process inside your arteries. It starts with damage to the inner lining of the artery, often from high blood pressure, smoking, or too much LDL (bad) cholesterol. Once that lining is injured, LDL particles slip in and get trapped. Your body sends immune cells to clean up the mess, but instead of fixing it, they turn the area into a fatty, inflamed patch.
These patches grow slowly. They start soft and full of lipids, then become harder as calcium builds up. The most dangerous plaques aren’t the biggest ones-they’re the unstable ones. These have thin caps, lots of fat, and lots of inflammatory cells. They might only block 30% to 40% of the artery, but they’re like time bombs. A small tear can trigger a blood clot, suddenly cutting off blood to part of your heart. That’s what causes most heart attacks.
Stable plaques, on the other hand, are thicker and more calcified. They might block over 70% of the artery, causing predictable chest pain during exercise (stable angina). But they’re less likely to rupture. The real danger lies in the quiet, unseen plaques that don’t cause symptoms until they explode.
Who’s at Risk?
Not everyone with high cholesterol gets CAD. Risk isn’t just about one number-it’s a mix of things that stack up. The 2023 ACC/AHA guidelines break patients into three risk groups: low (<1% chance of heart attack or death per year), intermediate (1%-3%), and high (>3%).
High-risk features include:
- Diabetes
- History of heart attack, bypass surgery, or stents
- Heart failure, especially with preserved ejection fraction (HFpEF)
- Chronic kidney disease (eGFR under 60)
- Smoking
- High blood pressure
- Obesity (BMI over 30)
- Atrial fibrillation
Here’s the scary part: 60% of people with CAD have at least one high-risk feature. And 75% of all heart attacks happen in that group. That means if you have diabetes and high blood pressure, your risk isn’t just doubled-it’s multiplied. Even if your cholesterol looks okay, other factors can push you into the danger zone.
Age matters too. The risk climbs after 45 for men and 55 for women. But younger people aren’t safe. With rising obesity and sedentary lifestyles, CAD is showing up in people in their 30s and 40s more than ever before.

How Is It Diagnosed?
There’s no single test for CAD. Doctors piece together clues from your history, symptoms, and tests.
An electrocardiogram (ECG) is often the first step. It checks your heart’s electrical rhythm. If you’re having chest pain, an ECG might show signs of reduced blood flow. But if you’re feeling fine, it can look normal-even if you have serious blockages.
Stress tests are more telling. You walk on a treadmill or get medication to make your heart work harder while your heart activity is monitored. If your heart doesn’t get enough blood during stress, it shows up on the test. This helps find blockages that aren’t obvious at rest.
The gold standard is coronary angiography. A thin tube is threaded from your wrist or groin to your heart. Dye is injected, and X-rays show exactly where the arteries are narrowed. It’s invasive, but it gives the clearest picture. Doctors use it when they’re sure you need intervention-or when a stress test is unclear.
Some patients also get an Ankle-Brachial Index (ABI) test. It measures blood pressure in your ankle compared to your arm. A low ratio suggests peripheral artery disease, which often goes hand-in-hand with CAD. If you have blocked leg arteries, you likely have blocked heart arteries too.
Treatment: Lifestyle, Medication, and Procedures
Treatment isn’t one-size-fits-all. It’s layered, starting with what you can do yourself-and adding more if needed.
Lifestyle changes are the foundation. No medication can replace quitting smoking, eating real food, moving daily, and managing stress. The Mediterranean diet-rich in olive oil, fish, nuts, vegetables, and whole grains-has been shown to reduce heart events by up to 30%. Walking 30 minutes a day, five days a week, cuts your risk of dying from CAD by nearly half.
Medications target the drivers of disease:
- Statins lower LDL cholesterol and stabilize plaques. Even if your numbers are "normal," many high-risk patients still need them.
- Aspirin helps prevent clots, but only for those with confirmed CAD or high risk. It’s not for everyone.
- Beta-blockers reduce heart rate and blood pressure, easing chest pain.
- ACE inhibitors or ARBs protect the heart after a heart attack or in people with diabetes or heart failure.
- GLP-1 agonists and SGLT2 inhibitors, originally for diabetes, now show strong heart protection-even in non-diabetics.
Some people need more than pills. Two main procedures help restore blood flow:
Percutaneous coronary intervention (PCI) is a minimally invasive procedure. A balloon is inflated inside the blocked artery, and a metal mesh stent is left behind to keep it open. It’s fast, often done the same day as diagnosis, and helps relieve chest pain quickly.
Coronary artery bypass grafting (CABG) is open-heart surgery. A vein or artery from another part of your body is used to create a detour around the blocked section. It’s more serious than PCI, but for people with multiple blockages or diabetes, it lasts longer and improves survival.
What About New Advances?
The 2023 guidelines are a game-changer. They don’t just treat blockages-they focus on preventing them from ever becoming dangerous. Risk stratification is now central. If you’re in the high-risk group, your treatment isn’t just about lowering cholesterol. It’s about stopping inflammation, stabilizing plaques, and protecting your whole cardiovascular system.
One emerging area is cardio-oncology. More people are surviving cancer, but some treatments damage the heart. At the same time, many cancer patients have undiagnosed CAD. Specialists now work together to manage both conditions safely.
Research is also exploring new drugs that directly target plaque inflammation. Early trials show promise in reducing heart attacks without increasing bleeding risk-a big problem with current anti-clotting drugs.
Living With CAD
If you’ve been diagnosed, it’s not a death sentence. But it’s a lifelong condition. You can’t just take a pill and forget about it. You need to stay active, eat well, take your meds, and keep up with checkups. Many people feel better after a stent or bypass and think they’re "cured." They stop exercising, go back to junk food, and skip medications. That’s when things go wrong.
Cardiac rehab programs are proven to cut death rates by 25%. They’re not just exercise classes-they’re education, nutrition coaching, and mental health support all in one. Yet, fewer than 30% of eligible patients enroll.
Don’t wait for symptoms. If you have risk factors-even if you feel fine-talk to your doctor. Get screened. Know your numbers. Your heart doesn’t warn you before it fails. But you can stop it before it gets there.
Final Thoughts
Coronary artery disease isn’t inevitable. It’s preventable. And if you already have it, you can still live a full, active life. The key is understanding how it works, knowing your personal risk, and acting early. It’s not about being perfect-it’s about being consistent. One healthy meal. One walk. One day of not smoking. Those add up. And they save lives.

15 Responses
This is the same propaganda the pharmaceutical lobby pushes to keep you hooked on statins. Atherosclerosis isn't caused by cholesterol-it's caused by chronic inflammation from processed sugars and seed oils. The real scandal? They never mention that countries with the highest butter and saturated fat intake have the lowest CAD rates. The data is rigged.
Thank you for this comprehensive and clinically accurate overview. It is rare to encounter such a well-structured summary that balances scientific rigor with public accessibility. The emphasis on plaque stability over mere stenosis is particularly insightful and aligns with current cardiology paradigms.
Did you know the FDA approved statins after a secret meeting with Big Pharma in 1987? They buried the data showing increased cancer rates. And why do all the 'experts' only talk about LDL? What about the 40% of heart attack patients with normal cholesterol? The system is designed to keep you dependent.
This is exactly the kind of clarity we need. I’ve been telling my patients for years that CAD isn’t about being ‘bad’-it’s about being informed. The Mediterranean diet isn’t trendy, it’s proven. And cardiac rehab? It’s not optional-it’s life insurance. If you’re reading this and have risk factors, please, just start walking. Today.
The nuanced distinction between stable and vulnerable plaques is, in my view, the single most underappreciated concept in preventive cardiology. One cannot adequately address a disease without understanding its biological architecture; to reduce CAD to a lipid disorder is to mistake the symptom for the syndrome. The inflammatory cascade-mediated by IL-6, TNF-alpha, and CRP-is the true engine, and until we target it with precision, we remain in the Stone Age of treatment.
Bro, this is gold. I’m from Delhi and my uncle had a heart attack at 42. He thought he was fine because he didn’t smoke. But he ate samosas daily, slept 4 hours, and drank chai with 5 spoons of sugar. This post? It’s the wake-up call India needs. Start walking. Stop sugar. Your heart doesn’t care about your Instagram diet.
I’m a nurse in Phoenix. I see this every day. People get a stent, go home, and think they’re fixed. Then they’re back in six months with another blockage. You don’t fix a lifetime of neglect with a metal tube. Lifestyle isn’t a suggestion-it’s the treatment. And yes, it’s hard. But you’re worth it.
It’s fascinating how the medical establishment has pathologized aging and metabolic adaptation into a disease of cholesterol, when in evolutionary terms, the human body was designed to store fat during scarcity and burn it during exertion. The modern environment-chronic caloric surplus, sedentary behavior, circadian disruption, and psychosocial stress-creates a perfect storm for endothelial dysfunction. The plaque is not the problem; it’s the symptom of a civilization that has lost its biological rhythm.
You think this is bad? Wait till you hear about the heart stents that were proven to be useless in 2017 but still get implanted 800,000 times a year because hospitals make $20k per procedure. And don’t even get me started on how the American Heart Association takes Big Pharma money. You’re being sold a bill of goods. Eat butter. Lift weights. Stop listening to doctors who’ve never run a marathon.
The current paradigm is fundamentally flawed. We’re hyper-focused on LDL-C as a biomarker while ignoring remnant cholesterol, Lp(a), and oxidized phospholipids. The 2023 ACC/AHA guidelines still rely on the Friedewald equation, which is mathematically invalid in hypertriglyceridemic states. We need lipidomics, not just panels. And we need to stop treating CAD like a plumbing issue.
statins cause diabeties and the heart attack thing is a lie. they inject you with microchips through the catheter. they track you. the cadiac rehab is a cover for mind control. i know because i read the documents. the dye? its nanotech. they want to control your heart rate remotely. dont trust the hospital.
Honestly, if you’re relying on a treadmill stress test to detect CAD, you’re already behind. Real medicine doesn’t wait for symptoms. Real medicine knows that a 35-year-old with a BMI of 32 and a fasting glucose of 102 is already in the danger zone. If you’re not getting a coronary calcium scan by 40, you’re gambling with your life-and frankly, you’re not thinking like an adult.
So… you’re telling me I need to stop eating pizza and start walking? Wow. Groundbreaking. Next you’ll tell me the sun rises in the east.
In my village in Nigeria, we don’t have statins. We have bitter leaf, moringa, and daily walking to the market. Our elders don’t die of heart attacks-they die of old age. The West turned a natural process into a medical industry. Maybe the cure isn’t in a pill, but in returning to how humans lived for 99% of our history.
i read this in class today and my prof said its good but i dont get why the plaques are unstable? like what makes them burst? can someone explain? ty