For many people with moderate to severe COPD, breathing doesn’t just get harder over time-it becomes a daily battle. Frequent flare-ups, or exacerbations, can send you to the hospital, wreck your schedule, and chip away at your quality of life. If you’ve been on a LAMA/LABA inhaler and still get sick two or more times a year, there’s a treatment option that’s changed the game: triple inhaler therapy. But it’s not for everyone. Understanding who benefits most-and who might be harmed-is critical.
What Exactly Is Triple Inhaler Therapy?
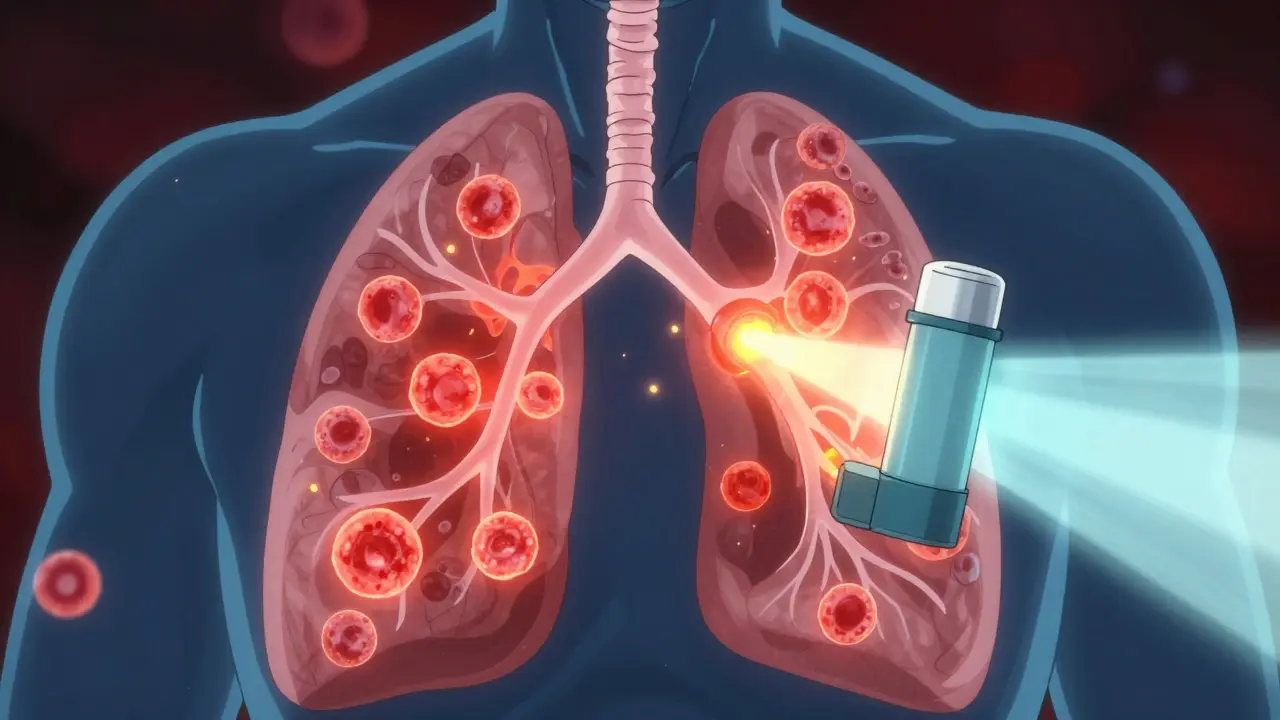
Triple inhaler therapy combines three types of medications in one device or two separate ones. It includes:- ICS (inhaled corticosteroid): Reduces airway inflammation
- LAMA (long-acting muscarinic antagonist): Opens airways by blocking muscle tightening
- LABA (long-acting beta-2 agonist): Relaxes airway muscles for easier breathing
Together, they tackle three root problems of COPD: swelling, narrowing, and mucus buildup. The goal isn’t just to manage symptoms-it’s to prevent flare-ups before they start.
There are two main ways to get this combo:
- Single-inhaler triple therapy (SITT): One device delivers all three drugs. Examples: Trelegy Ellipta (fluticasone furoate/umeclidinium/vilanterol), Trimbow (budesonide/glycopyrronium/formoterol)
- Multiple-inhaler triple therapy (MITT): You use three separate inhalers-one for each drug
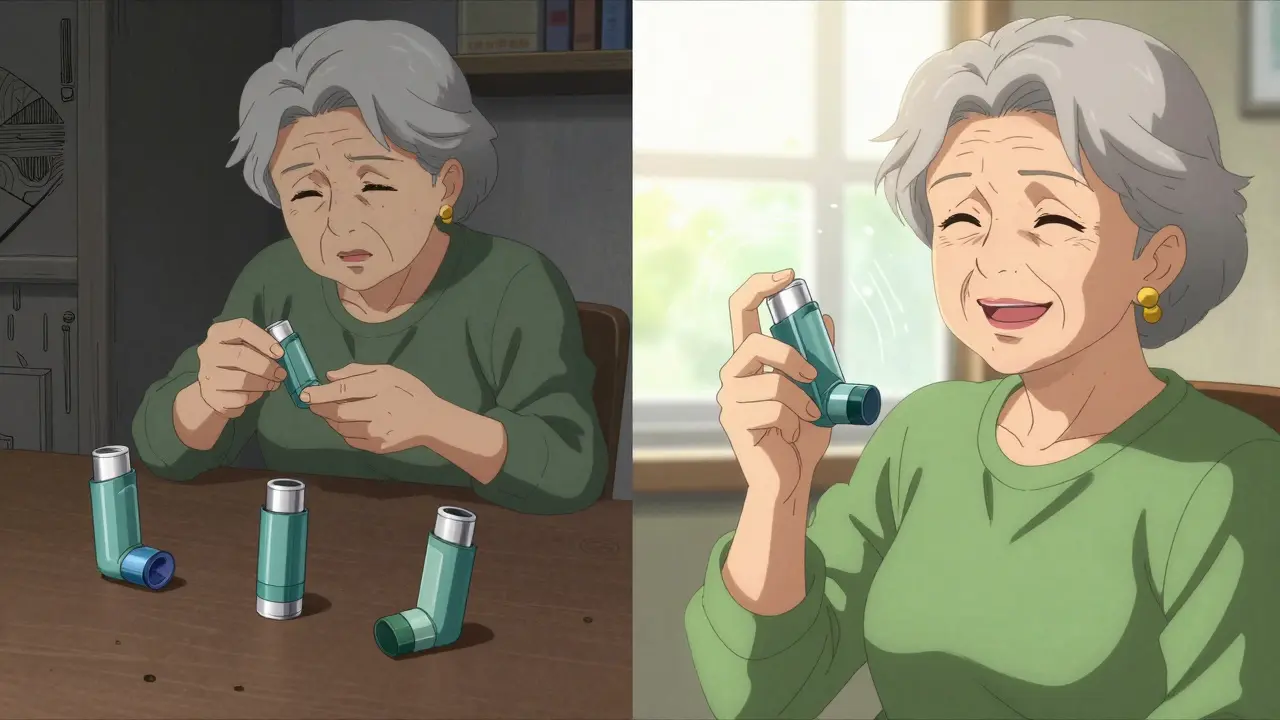
SITT is now the standard because it’s simpler. People who switch from MITT to SITT report fewer missed doses and fewer flare-ups. Why? Because carrying one device instead of three makes it easier to stick with the treatment.
Who Actually Benefits From Triple Therapy?
Not every COPD patient needs this. In fact, using triple therapy when you don’t need it can do more harm than good.The 2024 GOLD guidelines say triple therapy should only be considered if you meet two key criteria:
- You’ve had two or more moderate exacerbations in the past year, or one severe exacerbation that landed you in the hospital
- Your blood eosinophil count is 300 cells/µL or higher
Eosinophils are white blood cells that signal inflammation. High levels mean your airways are reacting strongly to triggers like infections or pollution. That’s where ICS-the anti-inflammatory part of triple therapy-makes the biggest difference.
Studies show patients with eosinophils ≥300 get about a 25% reduction in exacerbations compared to dual therapy. That’s not small. It means fewer emergency visits, fewer antibiotics, and more days you can actually do what you want.
But if your eosinophil count is below 100, triple therapy offers almost no benefit-and increases your risk of pneumonia. That’s why doctors now test your blood before prescribing it.
How It Compares to Other Treatments
Many people start with a LAMA/LABA combo-two bronchodilators that open the airways. It’s effective for many. But if you’re still getting sick, adding ICS can make a difference.Here’s how triple therapy stacks up:
| Therapy Type | Exacerbation Reduction | Pneumonia Risk | Adherence Rate | Best For |
|---|---|---|---|---|
| LAMA/LABA (dual) | Baseline (0%) | Low | 65-70% | Patients with infrequent exacerbations |
| Triple (SITT) | 15-25% | Medium to High | 78% | Eosinophil-high, frequent exacerbators |
| Triple (MITT) | 15-25% | Medium to High | 62% | Same as SITT, but less ideal |
Real-world data shows that while clinical trials show triple therapy reduces exacerbations by 15%, some observational studies suggest the benefit might be smaller-especially if patients were already on ICS before switching. That’s because when you stop ICS abruptly, your risk of flare-ups goes up temporarily. So the real win is when triple therapy is started properly, not when it replaces another treatment too quickly.
The Pneumonia Risk You Can’t Ignore
This is the biggest downside. Inhaled steroids suppress the immune system in your lungs. That’s good for inflammation-but it also makes it easier for bacteria to take hold.Fluticasone-based triple inhalers (like Trelegy) carry a higher pneumonia risk than budesonide-based ones (like Trimbow). One study found patients on fluticasone had an 83% higher chance of pneumonia than those on budesonide.
That’s why guidelines now say: if you’re over 65, smoke, have had pneumonia before, or have low eosinophils-triple therapy might not be worth the risk.
Doctors watch for signs like new or worsening cough, fever, or greenish mucus. If you’re on triple therapy, you should have a check-up every 3-4 months to monitor for this.
Why Adherence Matters More Than You Think
Medication only works if you take it. And with COPD, missing doses can lead to flare-ups within days.A study of 1,810 patients found that 68% of those using multiple inhalers missed at least one dose a week. Common reasons? Forgetting which one to use, getting confused about timing, or just finding it too cumbersome.
When patients switched to single-inhaler therapy, adherence jumped from 62% to 78%. That’s not just a number-it’s 16% fewer people ending up in the ER.
People who use SITT say things like, “I don’t have to carry three things in my bag,” or “I just do it once in the morning and forget about it.” Simplicity saves lives.
Cost and Access Are Real Barriers
The good news? Triple inhalers are more effective for the right people. The bad news? They’re expensive.In the U.S., brand-name SITT like Trelegy Ellipta can cost $75 to $150 per month out of pocket. Even with Medicare, many patients skip doses because they can’t afford them. One study found 22% of Medicare beneficiaries on triple therapy admitted to rationing their medication.
Generic versions aren’t available yet. Some insurers require prior authorization or step therapy-you have to try cheaper options first. That delay can mean more flare-ups while you wait.
If cost is an issue, talk to your doctor about patient assistance programs, manufacturer coupons, or whether a lower-cost dual therapy might still work for you.
What You Need to Do Next
If you’re on COPD maintenance therapy and still getting sick:- Check your eosinophil count. Ask your doctor for a recent blood test result. If it’s below 100, triple therapy won’t help.
- Review your exacerbation history. Have you had two moderate or one severe flare-up in the past year?
- Get your inhaler technique checked. Up to 70% of people don’t use their inhalers correctly. A simple demo from a nurse can make a huge difference.
- Ask about switching to SITT. If you’re on multiple inhalers, ask if a single-device option is right for you.
- Monitor for pneumonia. If you get a new cough, fever, or feel worse than usual, call your doctor right away.
Triple therapy isn’t a magic bullet. But for the right person-someone with frequent flare-ups and high eosinophils-it’s one of the most powerful tools we have to keep them out of the hospital and living better.
What’s Next in COPD Treatment?
The future of COPD care is getting more personal. Researchers are testing new biomarkers like fractional exhaled nitric oxide (FeNO) to see if it can predict who responds to ICS better than eosinophils.Biologics-drugs that target specific immune pathways-are also on the horizon. Dupilumab, originally for asthma and eczema, is now being tested in COPD patients with high eosinophils. Early results suggest it might reduce exacerbations without the pneumonia risk of steroids.
By 2027, doctors may be using blood tests and breathing tests together to pick the exact right treatment for each patient-no more guessing.
For now, the message is clear: triple therapy saves lives-but only when used precisely, carefully, and with full awareness of the risks.
Is triple inhaler therapy right for all COPD patients?
No. Triple therapy is only recommended for patients with moderate-to-severe COPD who have had two or more moderate exacerbations or one severe exacerbation in the past year AND have a blood eosinophil count of 300 cells/µL or higher. For patients with low eosinophil counts or infrequent flare-ups, triple therapy offers little benefit and increases the risk of pneumonia.
What’s the difference between Trelegy and Trimbow?
Trelegy Ellipta contains fluticasone furoate, umeclidinium, and vilanterol, and is taken once daily. Trimbow contains budesonide, glycopyrronium, and formoterol, and is taken twice daily. Budesonide-based Trimbow has a lower risk of pneumonia than fluticasone-based Trelegy. Trimbow also uses extrafine particles that may reach deeper into the lungs, which some studies suggest improves effectiveness.
Can I stop using my triple inhaler if I feel better?
No. COPD is a chronic condition, and triple therapy works to prevent flare-ups, not just treat symptoms. Stopping it suddenly can lead to a rebound in inflammation and a higher chance of severe exacerbations. Always talk to your doctor before making any changes.
Why do I need a blood test before starting triple therapy?
Blood eosinophil levels help predict whether the steroid component of triple therapy will help you. If your count is below 100 cells/µL, the steroid won’t reduce your flare-ups-but it will still raise your risk of pneumonia. Testing ensures you only get the treatment that will actually benefit you.
How do I know if I’m using my inhaler correctly?
Many people-up to 70%-use their inhalers wrong. Ask your doctor or pharmacist to watch you use it. You can also request a technique checklist or watch a video from the manufacturer. If you’re still having symptoms despite taking your meds, poor technique is a likely culprit.
Are there cheaper alternatives to brand-name triple inhalers?
Currently, no generic versions of single-inhaler triple therapy are available in the U.S. However, some patients can reduce costs through manufacturer coupons, patient assistance programs, or insurance prior authorization. If cost is an issue, ask your doctor if switching from multiple inhalers to a single device might still be affordable, or whether a different dual therapy might work for you.
What to Watch For
If you’re on triple therapy, keep an eye out for:- New or worsening cough, especially with fever or colored mucus
- Increased shortness of breath without a clear trigger
- Unexplained fatigue or loss of appetite
- More frequent use of rescue inhalers
These could signal pneumonia or a worsening of COPD. Don’t wait. Call your doctor.
Triple inhaler therapy is a powerful tool-but like any tool, it only works when used the right way. The goal isn’t just to take more medicine. It’s to take the right medicine, at the right time, for the right person.


9 Responses
My dad’s on Trelegy and he swears it cut his ER trips in half but he also got pneumonia last winter and it scared the hell out of us
Man I live in Delhi and the air here is basically a chemical soup so I get flare-ups every other month. Doc put me on triple therapy and honestly it’s been a game changer. I can actually walk to the market now without feeling like I’m running a marathon. But yeah the cost? Oof. I’m on a subsidy program through the hospital and it’s still a stretch. If you’re in India and struggling, ask about the government’s COPD support scheme - it’s not perfect but it helps. Also - don’t skip the eosinophil test. Mine was 420 and I was shocked. Turns out my body’s screaming for steroids. If yours is low? Don’t waste your money. I’ve seen guys on this stuff just because their doc pushed it and they ended up in the ICU with pneumonia. It’s not magic. It’s medicine. Use it smart.
For anyone thinking about switching to SITT - just do it. I was on three separate inhalers for a year. I’d forget which one did what, mix up the timing, and end up skipping days. When I switched to Trelegy, my adherence went from 50% to 90%. No joke. I started taking it right after brushing my teeth and now it’s just part of my routine. Also - get your technique checked. I thought I was doing it right until my nurse showed me I was puffing too fast. One demo changed everything. You don’t need to be a genius to use it - just consistent.
So I’m a respiratory therapist and I’ve seen this play out a hundred times. Triple therapy isn’t a upgrade - it’s a targeted intervention. Eosinophils above 300? You’re likely eosinophilic inflammation dominant. That’s your sweet spot. Below 100? You’re more of a neutrophilic or mixed phenotype - ICS is useless and just increases infection risk. And yes - fluticasone is worse than budesonide for pneumonia. Why? Particle size and lung retention. Budesonide’s extrafine particles clear faster. Also - if you’re over 65 and smoke? Triple therapy is a gamble. Not worth it. And don’t even get me started on the insurance hurdles. Prior auth takes weeks. People get sicker waiting. We need better access. Not just better meds.
Everyone’s acting like this is some miracle drug. It’s not. It’s a steroid cocktail with a side of pneumonia risk. The studies are funded by pharma. The guidelines are written by guys who get paid by the same companies. And don’t even get me started on the cost. You’re paying $150 a month for a device that’s just three drugs in one shell. The real solution? Quit smoking. Get pulmonary rehab. Stop relying on pills to fix a lifestyle disaster. This is corporate medicine selling dependency. If you’re still smoking and taking triple therapy you’re just buying time - not healing.
I’ve been on Trimbow for 8 months and honestly? I feel like I got my life back. I’m gardening again. I’m playing with my grandkids. I used to dread winter. Now I just bundle up and go out. The only thing that sucks? The twice-daily dosing. I wish it was once like Trelegy. But I’m not taking fluticasone after reading that pneumonia stat. I’d rather take it twice a day and live. Also - my doc didn’t even test my eosinophils at first. I had to ask. Don’t let them guess. Demand the blood test. It’s not complicated. It’s a simple CBC with differential. Ask for it. You’re worth it.
Oh wow. So let me get this straight. You’re telling me that if I’m poor, old, and Indian - and I smoke - I should just... die quietly? Because the steroid in my inhaler might give me pneumonia? And the only people who get this magic pill are the ones who can afford $150/month and have a fancy blood test? That’s not medicine. That’s a lottery. And the real joke? The same companies that make these inhalers also sell the antibiotics we need when we get pneumonia from their inhalers. Classic. I’m just waiting for the ad: "Trelegy - because pneumonia is just a side effect of living better."
Have you all considered that this is all part of a larger agenda? The WHO, CDC, and Big Pharma are pushing triple therapy to increase surveillance. The inhalers have microchips. They track your breathing patterns. Your location. Your medication adherence. And then they sell that data to insurance companies. That’s why they’re pushing the eosinophil test - it’s a backdoor to label you as "high risk" so they can raise your premiums. And the pneumonia risk? That’s not a side effect - it’s a feature. Less healthy people = more profits for hospitals. Wake up. This isn’t healthcare. It’s control.
Just wanted to say - if you’re reading this and you’re scared or confused - you’re not alone. I was diagnosed two years ago and I spent six months crying in my car after every doctor’s visit. I thought I was gonna die breathing into a plastic tube. Then I found a COPD support group online. People shared their stories - the good, the bad, the messy. I learned about eosinophils. I got my technique fixed. I switched to Trimbow because I didn’t want pneumonia. And now? I’m not cured. But I’m living. Not just surviving. Living. So if you’re out there feeling overwhelmed - take a breath. Ask one question. Talk to one person. You don’t have to figure it all out today. Just one step. That’s enough.