When your doctor prescribes a medication and the pharmacy says it’s out of stock - again - it’s more than just inconvenient. It’s disruptive. For some, it’s dangerous. Drug shortages in the U.S. hit 350+ times last year alone, and many of these aren’t temporary glitches. They’re systemic. When the pill you need isn’t made anymore, or it’s been pulled for quality issues, or it contains an ingredient you’re allergic to, you’re left with few options. One of them? Compounding pharmacies.
What Exactly Is a Compounding Pharmacy?
A compounding pharmacy isn’t your local CVS or Walgreens. It doesn’t just fill prescriptions from a bottle. It builds them from scratch. These pharmacies take raw ingredients - powders, liquids, chemicals - and mix them to make a medicine that doesn’t exist on store shelves. Think of it like a chef cooking a meal for someone with food allergies: no gluten, no dairy, no shellfish. Only here, it’s medicine tailored to your body.
They can turn a pill into a liquid for someone who can’t swallow. They can remove dyes or preservatives that trigger rashes. They can make a cream for pain relief instead of an oral pill that causes stomach issues. They can dose a child at 1.5 mg when the only commercial version comes in 10 mg. And they do it under strict rules - USP <795> for non-sterile mixes, USP <797> for sterile ones like injections or IVs.
There are about 7,500 specialized compounding pharmacies in the U.S., and another 32,000 offer some level of compounding. Most are small, independent shops, often run by pharmacists who’ve spent years learning how to safely blend ingredients without contamination. They’re not factories. They’re labs with gloves, hoods, and precision scales.
Why Do People Rely on Them?
Let’s say you’re a 72-year-old with severe arthritis. Your doctor wants you on a low-dose pain patch. But the only patch made contains lactose - and you’re allergic. The commercial version? Not an option. Your pharmacist calls a compounding pharmacy. They make you a custom transdermal gel with the exact dose you need, no lactose, no dyes, no fillers. You apply it once a day. Your pain drops. No stomach upset. No rash. That’s the real value.
Or you’re a parent whose 4-year-old needs antibiotics. The liquid version tastes like chalk. The child refuses to take it. The compounding pharmacist adds strawberry flavor, suspends the drug in a sugar-free base, and makes it thick enough to stay in the syringe. Adherence jumps from 40% to 80%. That’s not magic. That’s science.
For patients with hormone imbalances, chronic pain, or rare conditions, compounded meds are often the only way to get treatment. Studies show 85% of patients with allergies to commercial drug ingredients stick to their regimen when switched to compounded versions. That’s huge. Missing doses because of side effects or taste? That’s how hospitalizations start.
When Can’t They Help?
Compounding isn’t a magic wand. It can’t make biologics - things like insulin, monoclonal antibodies, or vaccines. These require complex biological processes you can’t replicate in a pharmacy lab. It can’t replace FDA-approved drugs just because they’re expensive or inconvenient. That’s dangerous.
Some doctors, well-meaning but misinformed, will write a prescription for a compounded version of a drug that’s actually available. A 2023 study found 15% of compounded prescriptions could’ve been filled with a regular pill. That’s unnecessary risk. Compounded meds aren’t tested in large clinical trials like FDA-approved drugs. They’re made batch by batch. Quality control is good - if the pharmacy is accredited - but it’s not the same.
The FDA is clear: compounding is for when there’s no other option. Not for convenience. Not for cost. Not because you don’t like the brand name.

How Do You Get One?
It starts with your doctor. They need to know a compounded option exists and agree it’s medically necessary. They’ll write a prescription that includes:
- The exact active ingredient
- The strength
- The dosage form (cream, liquid, capsule, etc.)
- Any excipients to exclude (e.g., “no gluten,” “no alcohol”)
- The reason (e.g., “allergic to FD&C Red #40”)
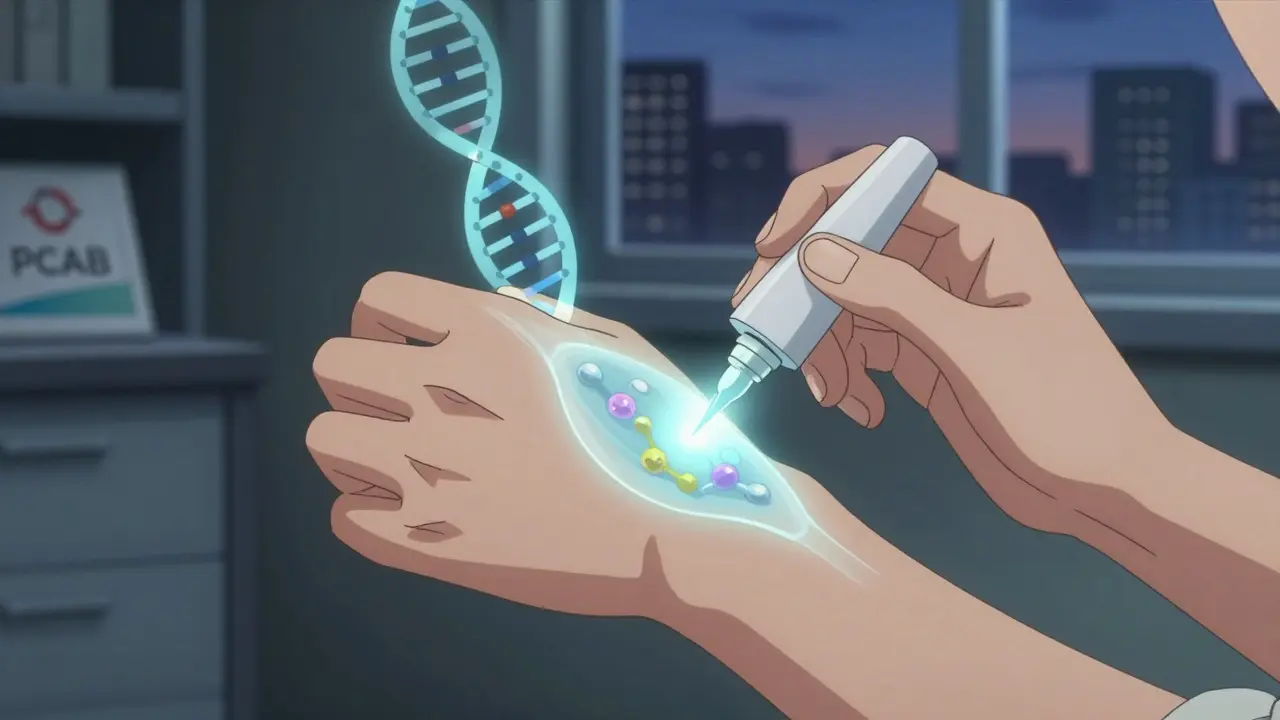
Then you find a pharmacy. Look for one accredited by the Pharmacy Compounding Accreditation Board (PCAB). Only about 1,200 out of 7,500 compounding pharmacies have this. It means they’ve passed independent audits for cleanliness, training, equipment, and record-keeping. You can search their database online.
Don’t just pick the cheapest one. Ask if they test their batches for potency and sterility. Ask how long the medication lasts. Ask about turnaround time - most take 24 to 72 hours. That’s longer than a regular fill, but it’s worth it if you’re stuck.
Cost and Insurance: What to Expect
This is the hard part. Most insurance plans don’t cover compounded meds the way they cover branded or generic drugs. About 45% of patients pay out of pocket. Some insurers will cover it if your doctor submits a letter of medical necessity. Others won’t touch it.
Costs vary. A simple flavored liquid might be $40-$80. A complex hormone cream or injectable could be $150-$300. Compare that to a $10 generic pill. It’s expensive. But for many, it’s the only way to stay healthy.
Some pharmacies offer payment plans. Some work with specialty pharmacy benefit managers. Ask. Don’t assume it’s impossible.
Real Stories, Real Impact
One Reddit user shared how their son had seizures triggered by dyes in seizure meds. After switching to a dye-free compounded version, seizure frequency dropped by 70%. Another person with chronic pain couldn’t tolerate oral opioids. A compounded topical gel let them manage pain without nausea or constipation. A woman with thyroid issues found the commercial version inconsistent - sometimes too strong, sometimes too weak. Her compounded version gave her stable levels for the first time in years.
These aren’t rare cases. They’re common enough that the compounding market is growing. It was worth $11.2 billion in 2022. By 2027, it’s expected to hit $15.8 billion. Why? Because drug shortages aren’t going away. And patients are demanding better solutions.
What’s Changing Now?
The FDA updated its guidance in 2022 to clarify when compounding is allowed during shortages. That’s good. It means more clarity for doctors and pharmacists.
Technology is helping too. New digital tools reduce compounding errors by 37%. Stability testing now extends shelf life by 25-40%. Some pharmacies are even starting to use genetic data to tailor meds - like adjusting a blood thinner dose based on a patient’s DNA. It’s early, but it’s happening.
Still, the system isn’t perfect. Waiting times are long. Insurance is a nightmare. And not every pharmacist has the training. That’s why accreditation matters. That’s why you ask questions.
Final Thoughts: Is It Worth It?
If you’ve been stuck because your medication isn’t available - or it makes you sick - then yes. It’s worth it. Compounding pharmacies fill a gap that big pharma won’t. They’re not perfect. They’re not cheap. But they’re often the only thing standing between a patient and no treatment at all.
Don’t give up when your pharmacy says, “We don’t have it.” Ask your doctor about compounding. Ask your pharmacist where to find a reputable one. You’re not asking for something unusual. You’re asking for the right medicine for your body. And that’s not too much to ask.
Are compounded medications safe?
Yes - if they’re made by an accredited pharmacy following USP standards. Compounded meds aren’t tested in large clinical trials like FDA-approved drugs, but they’re made under strict hygiene and quality controls. Look for PCAB accreditation. Avoid pharmacies that ship across state lines without proper licensing or don’t test their batches.
Can any pharmacy compound medications?
Technically, yes - many retail pharmacies offer basic compounding like flavoring liquids. But complex formulations - sterile injections, hormone creams, allergen-free capsules - require specialized training, equipment, and clean rooms. Only about 7,500 U.S. pharmacies are dedicated to advanced compounding. Don’t assume your local pharmacy can handle it.
How long does it take to get a compounded prescription?
Most take 24 to 72 hours. Sterile preparations (like injections) can take longer due to additional testing. Non-sterile ones like creams or flavored liquids are usually ready faster. Plan ahead - you can’t walk in and get it same-day like a regular refill.
Why don’t insurance companies cover compounded drugs?
Because they’re not mass-produced, FDA-approved products. Insurers base coverage on formularies - lists of approved drugs. Compounded meds don’t fit neatly into those lists. Some insurers will cover them with a letter from your doctor proving medical necessity, but many won’t. Be prepared to pay out of pocket.
Can a compounding pharmacy make a drug that’s been recalled?
Only if the recall was for manufacturing issues - not safety. If the active ingredient is safe and the problem was contamination or labeling, a compounding pharmacy can often recreate it. But if the drug itself is unsafe - like a recalled heart medication with a toxic impurity - they can’t legally make it. Always check with your pharmacist and doctor.


10 Responses
This whole compounding thing is just big pharma’s way of letting us rot while they jack up prices on generics. You think they care about your allergies? Nah. They’d rather you suffer than lose a patent. Compounding pharmacies are the only thing keeping people alive, and the FDA? They’d rather regulate a mom-and-pop shop than go after the corporations hoarding drugs. Wake up, people.
One must acknowledge, with due deference to the structural imperatives of pharmaceutical economics, that the proliferation of compounding pharmacies represents not a therapeutic innovation, but rather a symptomatic response to the collapse of regulatory oversight and supply chain integrity. The fact that patients must resort to artisanal pharmaceutical preparation-however noble in intent-underscores a systemic failure of market-based healthcare. One cannot help but lament the erosion of evidence-based medicine in favor of bespoke, unstandardized formulations.
Hey, just wanted to say this post gave me hope. I’ve been on a compounded thyroid med for 3 years now, and honestly? It’s the only thing that’s kept me from feeling like a zombie. I used to cry in the pharmacy aisle because nothing worked. Now I wake up and actually feel like myself. You’re not alone. There are people out there-pharmacists, doctors, patients-who are fighting for this. Keep asking. Keep pushing. You deserve to feel better. 🙌
It is noteworthy that the article does not address the regulatory disparities between state and federal oversight of compounding pharmacies. In the United States, while the FDA maintains jurisdiction over interstate commerce, intrastate compounding remains under the purview of state pharmacy boards, leading to significant variability in quality control. This fragmentation may explain why accreditation by PCAB is so critical. Further research into harmonization of standards would be beneficial.
My mate in Manchester had to get his asthma spray compounded after the brand got pulled. Took 3 weeks. Cost £180. But he’s breathing. So yeah, it’s a pain. But worth it. Simple as.
OMG YES. I got my kid’s ADHD med compounded because the regular one made him vomit. We went from ‘I hate school’ to ‘Can I go to soccer practice?’ in a week. The pharmacist even put in blueberry flavor. My wife cried. I cried. We all cried. This isn’t magic, it’s just… human. Stop acting like it’s some conspiracy. It’s medicine that actually works for people, not spreadsheets.
Compounding is just a workaround for lazy doctors and greedy pharmacists. If your kid can’t swallow a pill, give them a chewable. If they’re allergic, use a different drug. Stop treating patients like snowflakes.
How quaint. We’ve gone from ‘science’ to ‘chef’s special medicine.’ Next they’ll be adding glitter for mood enhancement. I’m sure the FDA’s 2022 guidance was just a cozy nap in a hammock made of regulatory loopholes. Truly, the pinnacle of modern healthcare: a pharmacist with a mortar and a dream.
I just wanted to say thank you for writing this. My mom’s been on a compounded pain cream for two years now. She can finally hold her grandkids again. It’s not perfect. It’s not cheap. But it’s real. And that matters more than any insurance form.
Thank you for sharing this. I’ve been trying to find a good compounding pharmacy for my dad’s hormone therapy, and honestly, I didn’t know where to start. The PCAB database was a lifesaver. I think more people need to know this exists. It’s not about being ‘alternative’-it’s about being human. I’m just glad there are people out there who care enough to make this happen. 🙏