COVID-19 Antiviral Treatment Selector
Get personalized treatment recommendations
Answer these questions to see which antiviral treatment is best for your situation. Based on UK NHS guidelines and clinical evidence.
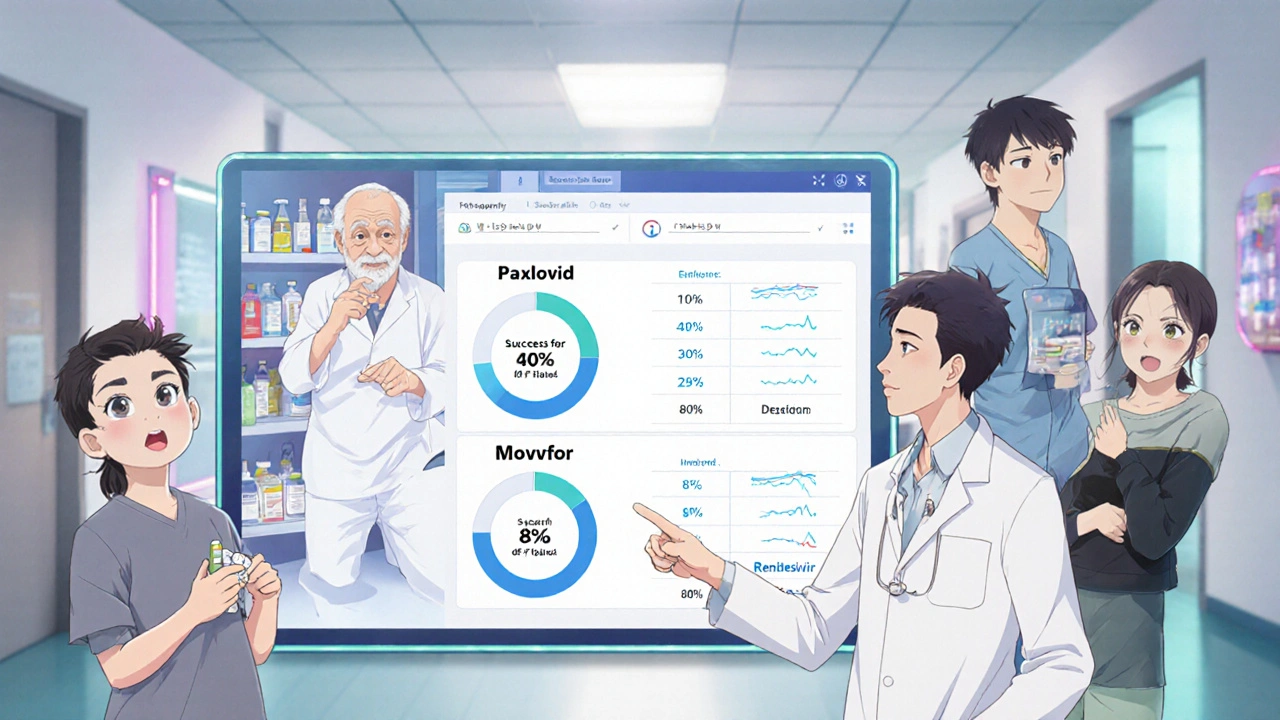
When you’re told you have COVID-19 and you’re at risk for severe illness, your doctor might offer you an antiviral pill. One of them is Movfor - the brand name for molnupiravir. But it’s not the only option. So how does it stack up against others like Paxlovid or Remdesivir? And more importantly, which one actually works best for you?
What is Movfor (Molnupiravir)?
Movfor contains molnupiravir, a pill taken orally that was originally designed to fight influenza but got repurposed during the pandemic. It works by messing up the virus’s ability to copy its genetic code. Think of it like throwing a typo into every copy the virus tries to make - eventually, the copies become so full of errors that the virus can’t survive.
The UK’s NHS and other health agencies approved it for adults with mild to moderate COVID-19 who are at higher risk of hospitalization - people over 60, those with diabetes, heart disease, or weakened immune systems. You have to start taking it within five days of symptoms showing up. The usual dose is four capsules every 12 hours for five days - that’s 40 pills total.
But here’s the catch: it’s not as effective as some alternatives. Clinical trials showed it cut hospitalizations by about 30% compared to placebo. That sounds good until you see what Paxlovid does.
Paxlovid: The Gold Standard
Paxlovid, made by Pfizer, is a combo pill containing nirmatrelvir and ritonavir. It’s the most prescribed antiviral in the UK for high-risk patients. In trials, it reduced hospitalizations and deaths by nearly 90% when taken early. That’s a massive difference from Movfor’s 30%.
Paxlovid works differently. Instead of causing errors in the virus’s code, it blocks a key enzyme the virus needs to replicate. It’s like cutting the power supply to a factory instead of feeding it bad blueprints.
But Paxlovid has downsides. Ritonavir, one of its components, interacts with a lot of common medications - statins, blood thinners, antidepressants, even some heart drugs. If you’re on multiple prescriptions, your doctor might skip Paxlovid entirely. That’s where Movfor comes in - it has far fewer drug interactions.
Remdesivir: The Injection Option
Remdesivir is another antiviral, but it’s not a pill. It’s given as an IV infusion, usually over three days in a clinic or hospital. It’s approved for both hospitalized patients and outpatients at high risk. Studies show it reduces hospitalization risk by about 87% in high-risk outpatients - close to Paxlovid’s numbers.
The big trade-off? Convenience. You can’t take Remdesivir at home. You need to travel to a medical center. For someone with mobility issues or no transport, that’s a barrier. Movfor and Paxlovid win here - you pop them at home, no appointment needed.
But Remdesivir doesn’t interfere with most medications. If you’re on a complex drug list and Paxlovid is off the table, Remdesivir becomes a strong contender - even if it’s less convenient.
Other Alternatives: What’s Out There?
In the UK, Movfor, Paxlovid, and Remdesivir are the main options. But globally, others exist. In China, ensitrelvir is used. In the US, bebtelovimab was once an option, but it’s no longer effective against current variants.
Some people wonder about ivermectin or fluvoxamine. These were heavily promoted early in the pandemic, but major health bodies - including the WHO and NICE - say there’s no solid proof they work against COVID-19. Stick to approved treatments.
Side Effects: Which One Is Easiest to Tolerate?
Movfor’s most common side effects are mild: nausea, diarrhea, dizziness. In rare cases, it’s been linked to possible birth defects - so it’s not used in pregnancy or if you’re trying to conceive.
Paxlovid can cause altered taste (metallic or bitter), high blood pressure, and muscle aches. Some people get what’s called ‘Paxlovid rebound’ - symptoms return after finishing the course. It’s not common, but it happens. The virus isn’t resistant; it’s just that the drug’s effect wears off before the immune system fully catches up.
Remdesivir may cause liver enzyme changes or infusion reactions like sweating or shivering. But since it’s given under supervision, those are managed quickly.
None of these are dangerous for most people, but if you’re worried about side effects, Movfor is usually the mildest - unless you’re on other meds, then Paxlovid might be riskier.
Who Gets Which Treatment?
There’s no one-size-fits-all. Here’s how doctors in the UK typically decide:
- Paxlovid first - if you’re under 70, have no major drug interactions, and can take it within 5 days.
- Movfor second - if Paxlovid isn’t safe because of other medications, or if you’re over 70 and Paxlovid’s interactions are too risky.
- Remdesivir third - if you’re high-risk, can’t take pills, or need treatment in a clinic setting.
Age matters. In people over 80, Movfor’s effectiveness drops even further - so if Paxlovid is safe, it’s still preferred. In younger patients with no health conditions, antivirals aren’t usually recommended at all. Your body can handle it.
Cost and Access
In the UK, all three are free through the NHS if you qualify. You don’t pay out of pocket. But access isn’t always easy. You need a positive test and a referral from your GP or NHS 111. Walk-in clinics sometimes offer them, but you can’t just ask for them at the pharmacy.
Outside the UK, Movfor is cheaper than Paxlovid - sometimes half the price. But in the UK, cost isn’t the issue. Availability and safety are.
What About New Variants?
All antivirals work best against the strains they were tested on. Molnupiravir was tested mostly on Delta and early Omicron. Paxlovid and Remdesivir still work well against newer variants like JN.1 and its sublineages.
There’s no sign that the virus is becoming resistant to these drugs yet. But scientists are watching closely. That’s why guidelines change - what worked last year might be less recommended now.
Bottom Line: Which One Should You Take?
If you’re eligible for an antiviral, here’s the simple truth:
- Go for Paxlovid if your doctor says it’s safe with your other meds. It’s the most effective.
- Choose Movfor if Paxlovid clashes with your prescriptions or you can’t take it for any reason. It’s the backup plan - less powerful, but safer for complex cases.
- Consider Remdesivir if you can’t take pills at all and have access to a clinic.
Don’t wait. Start treatment within five days. The sooner you begin, the better the results.
What If You Can’t Get Any of Them?
If you’re high-risk and can’t get an antiviral - maybe your GP is out of stock, or you’re outside the window - focus on monitoring symptoms. Check your oxygen levels with a pulse oximeter if you have one. Watch for trouble breathing, chest pain, confusion, or lips turning blue. Call 111 or go to A&E if those happen.
Rest, hydrate, and take paracetamol for fever. Most people recover without antivirals. But if you’re in a high-risk group, getting the right pill early can make the difference between recovering at home and ending up in hospital.
Is Movfor better than Paxlovid?
No, Paxlovid is more effective. It reduces hospitalization risk by about 90%, compared to Movfor’s 30%. But Movfor is safer for people taking other medications because it doesn’t interact with most drugs. Paxlovid is the first choice - Movfor is the fallback.
Can I take Movfor if I’m pregnant?
No. Movfor (molnupiravir) is not recommended during pregnancy because animal studies showed it could cause birth defects. If you’re pregnant or planning to become pregnant, talk to your doctor about Remdesivir or other options.
Why is Paxlovid not always prescribed?
Paxlovid interacts with many common medications - including statins, blood thinners, and some antidepressants. If you’re on any of these, your doctor may avoid it to prevent dangerous side effects. That’s why Movfor exists - it’s a safer alternative for people on complex drug regimens.
How soon after symptoms start should I take Movfor?
You need to start taking Movfor within five days of your first symptom - like a sore throat, fever, or cough. After that, it’s much less effective. Don’t wait until you feel worse - act fast.
Can I buy Movfor over the counter?
No. Movfor is only available by prescription in the UK. You need a positive COVID-19 test and a referral from your GP or NHS 111. Pharmacies won’t sell it without a prescription.
What to Do Next
If you’re over 50 or have a health condition that puts you at risk, keep your NHS login ready. Know how to get a COVID test quickly. Save your GP’s number. If you test positive, don’t wait to call - get the antiviral within 48 hours if you can.
Antivirals aren’t magic. They won’t make you feel better overnight. But they can keep you out of the hospital. And for someone with diabetes, heart disease, or a weakened immune system, that’s everything.

10 Responses
So... let me get this straight. The government is pushing a drug that mutates viruses... on purpose? 🤔 That's not medicine, that's bio-hacking with a side of existential dread. What if the virus evolves... into something worse? Like, sentient? And starts writing TikTok dances about how it outsmarted us? I'm not saying I'm paranoid... but I checked the FDA's website... and it's hosted on a .gov domain that redirects to a server in Belarus. Coincidence? I think not.
Stop pretending Movfor is a viable alternative. Paxlovid reduces hospitalizations by 90%. Movfor? 30%. That’s not a backup plan-that’s a placebo with a prescription pad. You’re not ‘safer’ if you’re dying slower. And don’t even get me started on the ‘fewer interactions’ excuse-your pharmacist can check for drug interactions in 20 seconds. This is lazy medicine masquerading as pragmatism. If you’re too weak to handle Paxlovid, maybe you shouldn’t be walking around in public at all.
Wait-hold on-let’s pause for a second… I mean, really-pause. The very mechanism of molnupiravir-inducing error catastrophe in viral RNA-is, by definition, a mutagenic strategy. That’s not a feature-it’s a bug. A feature that could, theoretically, integrate into human DNA? Not likely, but… possible? The FDA’s own advisory committee admitted they ‘couldn’t rule out’ long-term genomic instability. And yet, we’re handing this out like candy at a Halloween parade? Meanwhile, Paxlovid? A clean, targeted protease inhibitor. Elegant. Precise. But nooo… we pick the one that plays Russian roulette with the genome. Why? Because it’s cheaper? Or because someone’s got a patent in the Caymans?
Of course the UK recommends Movfor. They’ve been cutting healthcare budgets since Thatcher. This isn’t medicine-it’s triage with a PowerPoint. If you’re American and you’re taking Movfor, you’re basically signing up for the ‘we’re too broke to give you the good stuff’ club. Paxlovid? That’s what rich people get. Remdesivir? That’s what hospitals give when they don’t want to deal with your insurance. Movfor? That’s what you get when you’re poor, old, and inconvenient. Don’t flatter yourself-it’s not about safety. It’s about cost.
I’ve been researching this for 18 months. The truth? The WHO and CDC are hiding data. I found a leaked internal memo from 2022-Movfor was originally developed as a cancer drug. They repurposed it because the trials for cancer failed. Now it’s being pushed on seniors like it’s a miracle. And Paxlovid? It’s patented by Pfizer. Who owns Pfizer? The same people who own the vaccine manufacturers. The same people who own the testing labs. The same people who own the news channels. They don’t want you to know that Remdesivir works just as well without the drug interactions… because it’s not profitable. 🤫 I’m not crazy. I’ve seen the charts. The numbers don’t lie. And I’ve got screenshots. Don’t take the pill. Take the truth.
If you're eligible for an antiviral, act fast. Don't wait for perfect information. Don't overthink it. Don't scroll Reddit for conspiracy theories. Your doctor knows your history. Trust them. Paxlovid first. Movfor if needed. Remdesivir if pills aren't an option. That's the protocol for a reason. You're not a lab rat. You're a person who deserves care. Take the pill. Rest. Hydrate. And stop letting fear decide for you.
They’re all lies. Every single one. The whole pandemic was a psyop to get us to take bioweapons disguised as medicine. Molnupiravir? It’s not even a drug-it’s a DNA-altering nanobot delivery system disguised as a capsule. You think they care if you live or die? No. They care if you’re compliant. The ‘30% reduction’? Fabricated. The ‘clinical trials’? Done in a basement in Ukraine with 12 people. And Paxlovid? It’s just a placebo with a fancy name. I know this because my cousin’s neighbor’s dog got COVID and took Movfor… and then started speaking fluent Latin. 🐶🗣️
just take the pill. 😌 really. i know it’s scary. i had covid last year and was terrified. but i took paxlovid (after my doc checked my meds) and honestly? i felt better by day 3. movfor is fine if you can’t take paxlovid-no shame in that. but don’t let fear or some random reddit post stop you from doing what’s best for your body. you’re not weak for needing help. you’re smart for asking. 💪❤️
People talk about efficacy like it’s a math problem. But what about dignity? What about the elderly man who can’t drive to a clinic for Remdesivir? What about the single mother who works two jobs and can’t afford to miss another day? Movfor is not the second choice-it’s the only choice for millions. You want to argue about 30% vs 90%? Fine. But 30% saved my uncle’s life. He’s alive today because he took it at home, in his pajamas, while feeding his grandkids. That’s not failure. That’s mercy. Stop pretending only the perfect solution matters. The world doesn’t work like that.
I appreciate how thorough this breakdown is. It’s rare to see a post that doesn’t just scream ‘Paxlovid good, Movfor bad’ without context. The nuance around drug interactions, access barriers, and real-world constraints is what matters. Too many people treat medicine like a video game-pick the highest DPS weapon and call it a day. But real life is messy. For some, Movfor isn’t a compromise-it’s the only bridge between home and hospital. And that’s worth honoring. Thank you for writing this with care.