When someone with celiac disease eats bread, pasta, or even a sip of beer, their immune system doesn’t just react-it attacks. Not the gluten itself, but the lining of their own small intestine. This isn’t a food allergy. It’s not indigestion. It’s an autoimmune disease, and it’s more common than most people realize. Around 1 in 100 people worldwide have it, and many don’t even know. The trigger? Gluten. The damage? Real, measurable, and often silent until it’s advanced.
What Happens Inside Your Body When You Eat Gluten With Celiac Disease
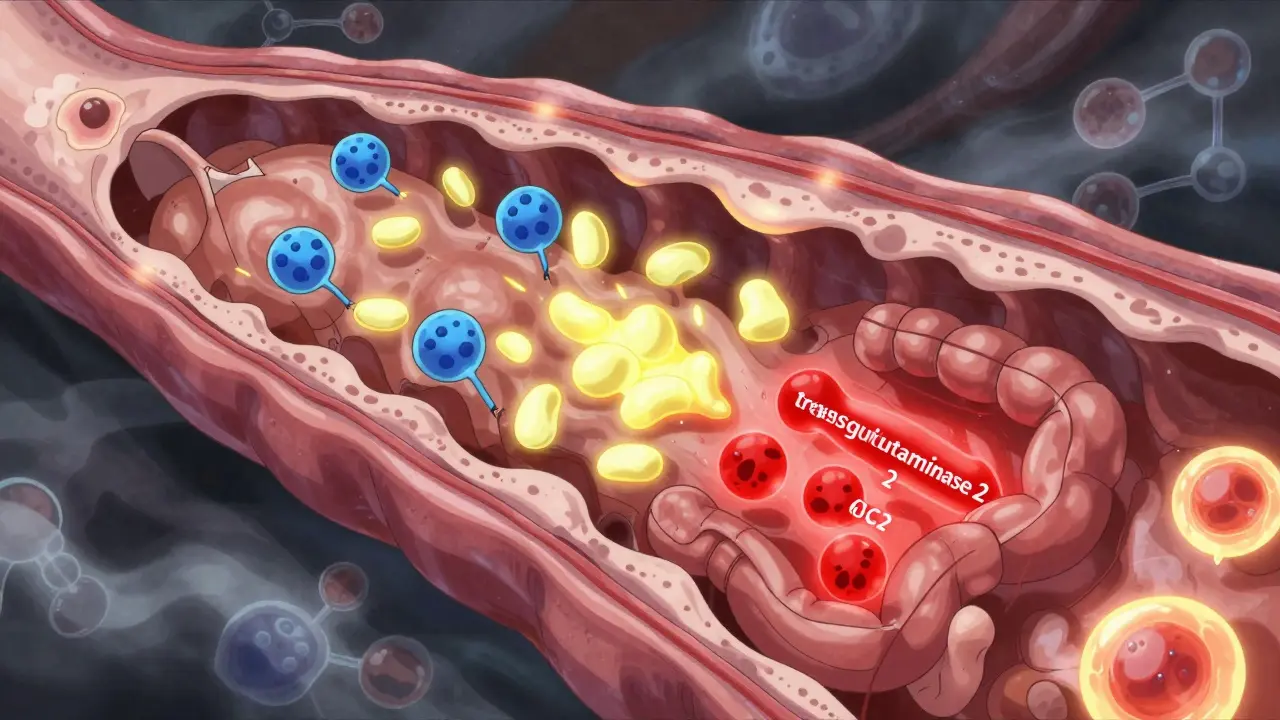
Celiac disease doesn’t just make you feel bloated or gassy. It’s a full-blown immune system malfunction. If you carry the HLA-DQ2 or HLA-DQ8 genes-which about 30% of people do-eating gluten can set off a chain reaction that turns your gut into a battleground. Gluten isn’t fully broken down in your stomach. Fragments like the 33-mer gliadin peptide slip through the intestinal lining. Normally, this wouldn’t be a problem. But in celiac disease, a protein called tissue transglutaminase 2 (TG2) modifies these fragments, making them stickier and more recognizable to your immune cells. These modified pieces then latch onto HLA-DQ2 or HLA-DQ8 molecules on immune cells in your gut wall. That’s the signal: “This is foreign. Attack.” Your immune system responds by sending in T-cells, especially CD4+ cells, which release inflammatory signals like interferon-gamma. These chemicals cause your intestinal villi-the tiny, finger-like projections that absorb nutrients-to flatten and shrink. This is called villous atrophy. The deeper crypts in your gut lining grow longer (crypt hyperplasia), and immune cells pile up between the cells lining your intestine. The result? Poor nutrient absorption, fatigue, weight loss, and sometimes no symptoms at all. A 2024 study from McMaster University changed how we think about this. It turned out the gut lining itself isn’t just a passive target. Cells in the epithelium, when they express the same HLA molecules as immune cells, can actually start the immune response on their own. This means your gut isn’t just being attacked-it’s helping to start the attack.Celiac Disease vs. Non-Celiac Gluten Sensitivity
Not everyone who feels bad after eating gluten has celiac disease. Many people report symptoms like brain fog, joint pain, or bloating without the intestinal damage. That’s non-celiac gluten sensitivity (NCGS). But here’s the key difference: celiac disease is measurable. NCGS isn’t. Celiac disease has clear diagnostic markers. The gold standard is a blood test for anti-tissue transglutaminase (tTG-IgA) antibodies. These are present in 98% of people with active celiac disease who are still eating gluten. A biopsy showing Marsh stage 2 or 3 damage confirms it. NCGS has no blood test, no biopsy pattern, and no genetic link. It’s diagnosed by elimination-remove gluten, feel better, reintroduce it, feel bad again. The immune response differs too. In celiac disease, your body produces IgG3 antibodies, indicating repeated immune activation without tolerance. In NCGS, IgG profiles suggest a different, less aggressive reaction. And while celiac patients must avoid gluten down to 20 parts per million (ppm)-the legal limit for “gluten-free” labeled foods-some with NCGS can tolerate small amounts without long-term damage.Why Diagnosis Takes So Long
The average time to diagnosis? Over six years. That’s not because doctors are slow. It’s because celiac disease doesn’t always look like classic diarrhea and weight loss. Many people have fatigue, anemia, joint pain, infertility, or even neurological symptoms like tingling in their hands. Others feel fine-until their next endoscopy reveals severe intestinal damage. A 2023 survey from the Celiac Disease Foundation found that 68% of patients waited more than five years for a diagnosis. One Reddit user shared they saw four different gastroenterologists over seven years before getting a biopsy that confirmed celiac disease. That delay isn’t rare. It’s the norm. Why? Because doctors still don’t routinely test for it. Many assume it’s IBS or stress. Even when symptoms point to malabsorption-low iron, low vitamin D, unexplained weight loss-celiac isn’t always the first thing checked. But if you have a family history, unexplained anemia, or autoimmune conditions like thyroid disease or type 1 diabetes, you should be tested.
The Only Treatment: A Strict Gluten-Free Diet
There is no cure. No pill. No vaccine. The only treatment right now is a lifelong, 100% gluten-free diet. And it’s harder than it sounds. Gluten hides everywhere. It’s in soy sauce, malt vinegar, some medications, lip balm, and even Play-Doh. A 2022 FDA report found that only 37% of prescription drugs list gluten content. Many people don’t realize their daily multivitamin or headache pill contains wheat starch. Cross-contamination is a huge issue. A toaster used for regular bread can leave enough gluten residue to trigger a reaction. A shared fryer, cutting board, or butter knife can be enough. One study found that using a dedicated gluten-free toaster reduced cross-contamination risk by 85%. The cost? It’s steep. Gluten-free products cost an average of 242% more than their regular counterparts. A box of gluten-free pasta might be $5.50. The regular kind? $2.20. For families, that adds up fast. And insurance rarely covers it. Only 12% of U.S. health plans help pay for gluten-free foods.What Success Looks Like
The good news? Most people feel dramatically better once they go gluten-free. The Celiac Disease Foundation survey showed that 89% of patients saw major improvement within six months. Symptoms like bloating, diarrhea, and fatigue fade. Iron and vitamin levels climb. Bone density improves. Skin rashes like dermatitis herpetiformis clear up. One user on Beyond Celiac forums shared that after five years of strict avoidance, their follow-up endoscopy showed complete mucosal healing. Their villi had regrown. Their body was finally absorbing nutrients again. But healing takes time. It can take 18 months to two years for the gut to fully recover in adults. In kids, it’s faster-often under six months. And even then, 30% of diagnosed adults still have symptoms despite a gluten-free diet. Why? Hidden gluten. Stress. Other food intolerances. Or maybe, as researchers suspect, something else we haven’t figured out yet.What’s on the Horizon
The future of celiac disease isn’t just about avoiding gluten anymore. Researchers are working on therapies that could change everything. - Nexvax2: A vaccine-like therapy using gluten peptides to retrain the immune system. Phase 2 trials in late 2023 showed a 42% reduction in symptoms. - Latiglutenase: An enzyme that breaks down gluten in the stomach before it reaches the intestine. The 2022 CeliAction trial showed 37% fewer symptoms. - TAK-101: A nanoparticle treatment that targets the immune response directly. In 2023, it cut intestinal damage by 63% in trial participants. These aren’t cures. But they might one day let people eat gluten occasionally without damage. Meanwhile, scientists are developing apps and devices that can detect gluten in food at levels as low as 5 ppm-far stricter than current labeling rules.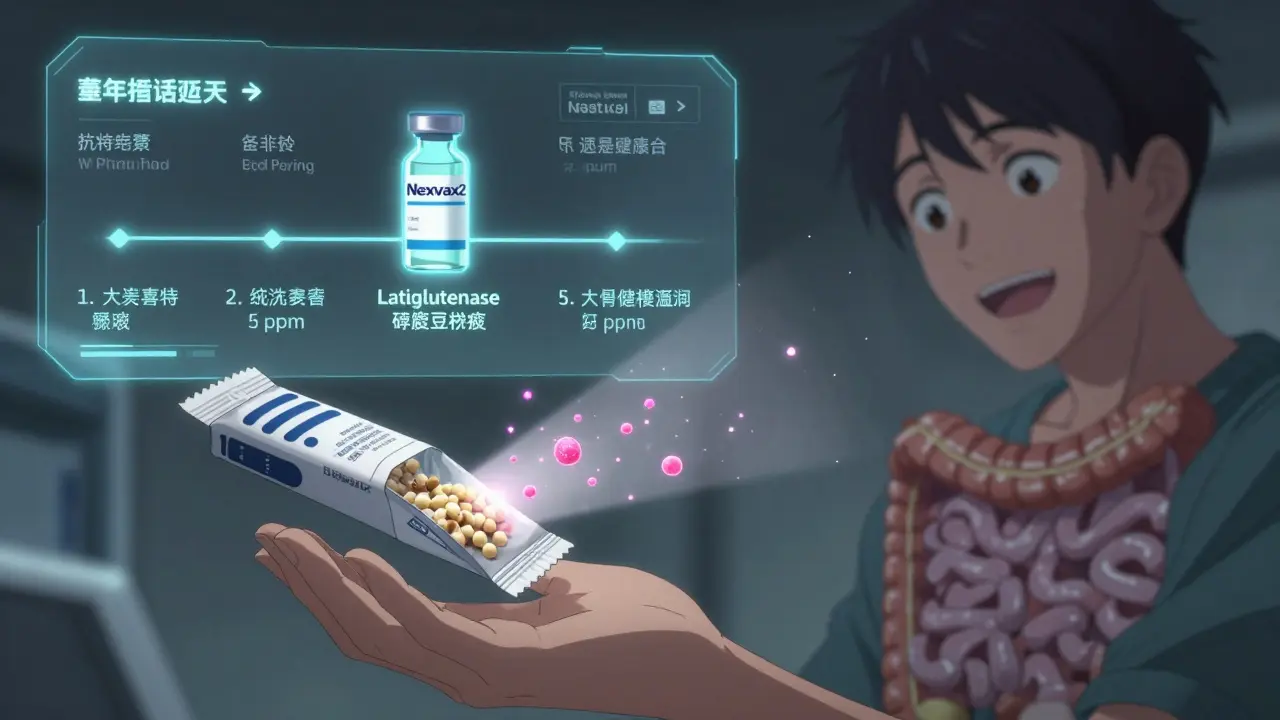
How to Get Started
If you’ve been diagnosed-or suspect you have celiac disease-here’s how to begin:- Clear your kitchen. Replace cutting boards, toasters, colanders, and utensils that have touched gluten. Use separate jars for butter, jam, and peanut butter.
- Learn to read labels. Look for “gluten-free” certification (GFCO, NSF). Watch for hidden gluten: malt, dextrin, modified food starch, hydrolyzed vegetable protein.
- Focus on whole foods. Rice, quinoa, corn, potatoes, fruits, vegetables, meat, eggs, and dairy (if tolerated) are naturally gluten-free.
- Carry snacks. Always have a gluten-free protein bar or nuts in your bag. Restaurant meals aren’t always safe.
- Test for deficiencies. Get checked for iron, ferritin, vitamin D, B12, and calcium. Most people with celiac are deficient.
- Use apps. Find Me Gluten Free has over 185,000 reviews and helps locate safe restaurants.
Frequently Asked Questions
Can celiac disease develop later in life?
Yes. While it often shows up in childhood, celiac disease can appear at any age. Many people are diagnosed in their 40s, 50s, or even later. Stress, infections, surgery, or pregnancy can trigger the disease in genetically predisposed people. The HLA-DQ2/DQ8 genes are present from birth, but the immune reaction only starts when something flips the switch-often decades later.
If I don’t have symptoms, do I still need to avoid gluten?
Absolutely. Even if you feel fine, eating gluten continues to damage your small intestine. Over time, this increases your risk of osteoporosis, infertility, neurological disorders, and even intestinal lymphoma. The damage is silent, but it’s real. A 2021 Mayo Clinic study found that 47% of celiac patients had vitamin D deficiency, and 33% had iron deficiency-even those who felt healthy.
Is a gluten-free diet healthy if you don’t have celiac disease?
Not necessarily. Gluten-free products are often lower in fiber, iron, and B vitamins because they’re made with refined flours instead of whole wheat. Many are also higher in sugar and fat to improve taste. Unless you have celiac disease or a confirmed gluten sensitivity, there’s no proven health benefit to avoiding gluten. In fact, cutting out whole grains without a medical reason can hurt your long-term heart and gut health.
Can I ever eat gluten again if my symptoms go away?
No. Celiac disease is lifelong. Even if your symptoms disappear and your blood tests normalize, reintroducing gluten will restart the immune attack and damage your gut again. Studies show that even tiny amounts-like crumbs from a shared toaster-can trigger inflammation and prevent healing. There’s no such thing as “too little” gluten if you have celiac disease.
How do I know if I’m still being exposed to gluten?
The best way is through regular blood tests. Anti-tTG antibody levels drop when you’re strictly gluten-free and rise again if you’re exposed. If your levels stay high despite a gluten-free diet, you’re likely still getting gluten from hidden sources. Some clinics now offer stool tests for gluten peptides, and new devices are being developed to detect gluten in food at home. But for now, blood tests and careful label reading are your best tools.

13 Responses
I went gluten-free last year after years of unexplained fatigue. Within 3 weeks, I felt like a different person. No more brain fog. No more afternoon crashes. It’s wild how something so simple can change everything.
i always thought celiac was just 'gluten intolerance' until i read this. holy crap. the part about TG2 modifying gliadin peptides? that's wild. i had no idea the body was literally reshaping the gluten to make it look foreign. my gut is now screaming at me to stop eating bread. lol.
you know what? in india we dont even have this problem because we eat mostly rice and lentils. why are westerners so obsessed with wheat? we have idli, dosa, upma, pongal-so many gluten-free options naturally. why do you even need bread? your diet is the problem, not the gluten. also, i tried gluten-free pasta once-it tasted like sawdust. stick to real food.
I’ve been living with this for 14 years. I’ve had three endoscopies. I’ve been to five different gastroenterologists. I’ve spent over $18,000 on gluten-free products. I’ve been mocked at family dinners. I’ve been told I’m 'just being dramatic.' And yet-when I finally got diagnosed, I cried. Not because I was sad. Because I was so damn tired of being told it was 'all in my head.' This isn’t a diet. It’s survival.
Thank you for this comprehensive and meticulously researched overview. The distinction between celiac disease and non-celiac gluten sensitivity is critically under-discussed in public discourse. The fact that villous atrophy can occur asymptomatically underscores the necessity of proactive screening in high-risk populations. I particularly appreciate the inclusion of the 2024 McMaster University findings regarding epithelial HLA expression-this represents a paradigm shift in our understanding of mucosal immunology.
people who say 'gluten-free is just a fad' clearly never had to read ingredient labels for 12 years. i’ve found gluten in lip gloss, soy sauce, and my dentist’s toothpaste. you think you’re safe? you’re not. and yes, i’ve cried in the grocery store because the gluten-free bread was $8.50 and my paycheck didn’t cover it. stop judging. you don’t know what it’s like.
I was diagnosed at 47 after a routine blood test revealed iron deficiency. My doctor didn’t even mention celiac. I had to push for it. Now, seven years later, I’m still adjusting. The worst part? People think 'gluten-free' means 'healthy.' It doesn’t. It just means 'not wheat.' I eat a lot of rice cakes and almond butter. I miss sourdough. But I’d rather live than eat bread.
If you're reading this and you think you might have celiac, please get tested before going gluten-free. Seriously. Once you cut it out, the tests won’t work anymore. I waited too long. I thought I had IBS. I had a biopsy that showed Marsh 3b. I wish I’d known sooner. You’re not alone. There are communities out there. You can live a full life. It’s just going to take some work.
in india we have so many traditional foods that are naturally gluten free like idli, dosa, pongal, upma, and even jowar roti. why are westerners so obsessed with wheat? we dont have this problem because we dont eat bread every day. also, gluten free products are so expensive here too. i wish there was a way to make them cheaper. maybe government subsidies? also, i tried the gluten free pasta and it tasted like plastic. i miss real pasta. but i cant have it. so i eat rice. its fine.
so let me get this straight. you’re telling me the government allows companies to put gluten in lip balm and Play-Doh? and then they label it 'gluten-free' at 20ppm? what kind of joke is this? next they’ll say it’s safe to eat gluten if it’s below 100ppm. then 500ppm. then 'gluten-free' just means 'not 100% wheat.' they’re gaslighting us. and don’t even get me started on the pharmaceutical industry-they don’t list gluten in meds because they don’t want to be sued. this is a conspiracy. i’ve been poisoned for 12 years. and no one cares.
I didn’t realize how much my joint pain was linked to gluten until I cut it out. My knees stopped aching. My hands stopped tingling. I didn’t even know I was sick. I just thought I was getting older. Now I feel like I got my 20s back. I still miss pizza. But I’d rather be pain-free.
wait-so if your gut cells express HLA-DQ2, they can start the immune response themselves? that’s insane. so it’s not just T-cells attacking? your own intestinal lining is like... turning traitor? that’s next level. i always thought it was just the immune system going rogue. but if the tissue itself is helping? that’s terrifying. and beautiful. in a horror-movie kind of way.
I got diagnosed after my third miscarriage. My OB didn’t even blink. Said, 'Try yoga.' I cried in the parking lot. Then I went home, threw out every piece of bread in the house, and cried again. But this time, it was because I finally knew why. I’m 33 weeks pregnant now. My baby’s healthy. My villi are healing. I’m not 'cured.' But I’m alive. And I’m not letting anyone tell me this is 'just stress.'