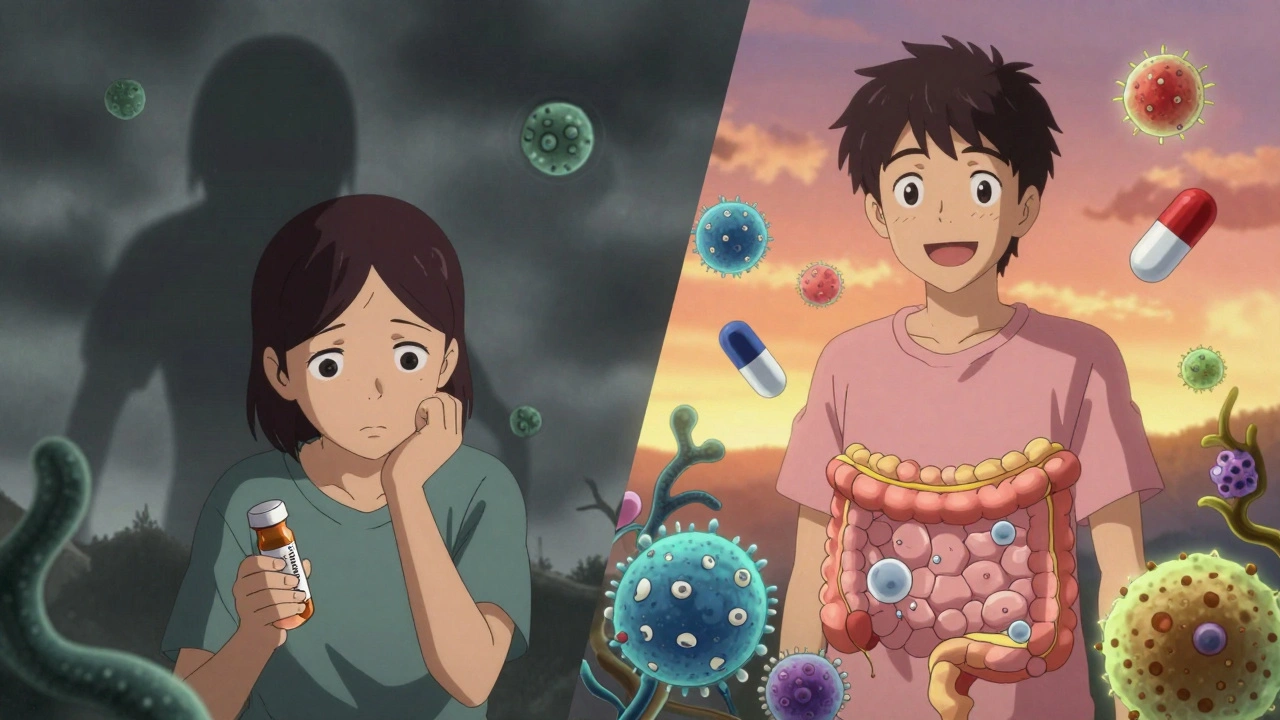
Most people don’t think about their gut bacteria until something goes wrong. Then, out of nowhere, they’re hit with relentless diarrhea, stomach cramps, and fever - often after a simple course of antibiotics. This isn’t just bad luck. It’s C. difficile colitis, a dangerous infection that’s become one of the most common hospital-acquired illnesses in the UK and US. And here’s the harsh truth: the very drugs meant to heal you can be the reason you get sicker.
How Antibiotics Trigger C. diff
Antibiotics don’t just kill the bad bacteria. They wipe out the good ones too - the trillions of microbes that live in your gut and keep harmful invaders like Clostridioides difficile in check. When that balance breaks, C. diff multiplies fast, releasing toxins that chew through the colon lining. The result? Severe diarrhea, fever, nausea, and in worst cases, colon rupture or sepsis.
The risk isn’t the same for every antibiotic. Some are far more dangerous than others. A 2023 study of over 33,000 hospital patients found that piperacillin-tazobactam, a broad-spectrum combo drug, carries the highest risk - nearly double the chance of triggering C. diff compared to other antibiotics. Carbapenems and later-generation cephalosporins like ceftriaxone are almost as bad. Even more surprising? Clindamycin, once a common go-to for dental or skin infections, is still one of the top offenders. It’s not just about strength - it’s about how deeply the drug disrupts the gut microbiome.
And it’s not just hospitals. Community cases are rising. About half of people who get C. diff never set foot in a hospital. They got it after a simple course of antibiotics at their GP’s office. One UK study found that nearly 50% of community C. diff patients had taken antibiotics within the past 30 days. The CDC calls this an "urgent threat" - and for good reason. In the US alone, it causes 500,000 infections and nearly 30,000 deaths each year. The UK sees tens of thousands of cases annually, with many going undiagnosed or mislabeled as "food poisoning."
Why Stopping Antibiotics Isn’t Always Enough
Doctors often tell patients: "Stop the antibiotic if you think it’s causing problems." But that’s easier said than done. If you’re being treated for pneumonia or a severe urinary tract infection, stopping too soon can lead to treatment failure - or worse, antibiotic-resistant bacteria. The trick is knowing when to stop.
Research shows the risk doesn’t spike right away. It creeps up. Each extra day on antibiotics increases your chance of C. diff by 8%. The danger really takes off after 14 days. That’s why NICE guidelines now push for antibiotic reviews within 48 to 72 hours. If the infection isn’t improving, switch or stop. If it is, cut the course short.
But here’s the catch: some people carry C. diff without symptoms. They’re silent carriers. For them, antibiotics don’t increase risk - they just wake up the bacteria already living inside. That’s why even "responsible" antibiotic use doesn’t protect everyone. And that’s why we need better tools.

Fecal Transplant: The Gut’s Reset Button
When standard treatments fail - and they often do - there’s a solution that sounds strange but works shockingly well: fecal microbiota transplantation, or FMT.
It’s not as gross as it sounds. Healthy donor stool is processed, filtered, and delivered into the patient’s colon. The goal? Rebuild a healthy gut ecosystem. Think of it like reseeding a lawn after a chemical spill. The bad bacteria are still there, but now they’re outnumbered by good ones that fight back.
The numbers speak for themselves. In a landmark 2013 trial published in the New England Journal of Medicine, 94% of patients with recurrent C. diff were cured after just one or two FMT treatments. Compare that to vancomycin, the standard drug treatment, which only worked in 31% of cases. Since then, multiple studies have confirmed FMT cures 85-90% of recurrent cases.
Delivery methods vary. Colonoscopy is the most common - about 65% of procedures. But oral capsules, frozen and carefully screened, are growing fast. They’re less invasive, easier to store, and just as effective. In the US, the FDA approved two branded FMT products in 2022 and 2023: Rebyota and Vowst. These aren’t "dirty poop" - they’re standardized, tested, and regulated. In the UK, FMT is still mostly done in hospitals under strict protocols, but the shift toward packaged therapies is coming.
Who Gets FMT - And Who Doesn’t
FMT isn’t for everyone. Guidelines from the American Gastroenterological Association and NICE say it’s for patients with three or more recurrences of C. diff. That’s because the first infection is usually treated with antibiotics like vancomycin or fidaxomicin. Fidaxomicin is more expensive than vancomycin, but it’s better at preventing relapse - it keeps the infection from coming back 90% of the time, compared to 86% with vancomycin.
For those who still relapse, FMT becomes the next step. Some patients have tried every antibiotic, even multiple rounds of vancomycin, only to see symptoms return weeks later. One Reddit user from Birmingham described going through five flare-ups over two years - each time, the same brutal diarrhea, each time, the same hospital visit. "I was ready to give up," they wrote. "Then I got FMT. Within three days, I felt normal again. No more fear of the toilet."
But FMT isn’t risk-free. There’s a small chance of transferring other infections - like drug-resistant bacteria or viruses - if donor screening isn’t thorough. That’s why all UK and US programs require donors to pass extensive blood and stool tests. Long-term effects? Still being studied. But so far, no major safety issues have emerged in thousands of treated patients.
What’s Next? Beyond the Poop
Scientists are working on cleaner, smarter alternatives. One promising candidate is SER-109, a pill made from purified bacterial spores from healthy donors. In a 2022 trial, it cured 88% of recurrent C. diff cases - almost matching FMT’s success, without the stigma. It’s already approved in the US and expected to arrive in the UK soon.
There’s also bezlotoxumab, a monoclonal antibody that neutralizes one of C. diff’s main toxins. Given as a single IV infusion alongside antibiotics, it cuts recurrence risk by 10%. It’s expensive - around £3,000 per dose - but for high-risk patients, it’s a game-changer.
And prevention? It’s still about antibiotics. Less is better. Narrow-spectrum drugs where possible. Shorter courses. Avoiding clindamycin and cephalosporins unless absolutely necessary. Hospitals in the UK are slowly adopting "Start Smart, Then Focus" programs - checking prescriptions within 72 hours and switching to targeted therapy.
The future isn’t just about treating C. diff. It’s about stopping it before it starts. That means better diagnostics, smarter antibiotics, and a deeper understanding of the gut microbiome. For now, though, if you’ve had C. diff more than twice, FMT isn’t just an option - it’s your best shot at getting your life back.
What You Can Do
- If you’re prescribed an antibiotic, ask: "Is this really necessary?" and "Is there a narrower-spectrum option?"
- Never stop antibiotics without talking to your doctor - but do ask if you can shorten the course.
- If you’ve had C. diff before, keep a record. Tell every doctor you see - even dentists.
- If you’ve had three or more recurrences, ask your GP or gastroenterologist about FMT.
- Don’t use probiotics to prevent C. diff. Studies show they don’t help - and in vulnerable people, they might even cause harm.
Can you get C. diff without taking antibiotics?
Yes, but it’s rare. Most cases are linked to recent antibiotic use. However, some people become carriers after exposure to contaminated surfaces or healthcare settings. Asymptomatic carriers can spread the bacteria without showing symptoms. Community-acquired cases are rising, especially among older adults and those with weakened immune systems, even without recent antibiotics.
Is fecal transplant safe?
When done through approved programs, FMT is very safe. Donors are screened for over 30 infectious diseases, including HIV, hepatitis, and drug-resistant bacteria. The risk of serious side effects is less than 2%. The most common issues are mild bloating or cramping after the procedure. Long-term data is still being collected, but no major safety concerns have emerged in over 10 years of use.
How effective is FMT compared to antibiotics?
For recurrent C. diff, FMT is far more effective. After one treatment, 81% of patients are cured. After two, that jumps to 94%. Standard antibiotics like vancomycin cure only about 31% of recurrent cases. Even the best antibiotic, fidaxomicin, has a recurrence rate of 14-19%. FMT cuts that risk to under 10%.
Are there alternatives to poop transplants?
Yes. In the US, FDA-approved oral products like Rebyota and Vowst use purified, processed donor stool in capsule form. Another option is SER-109, a pill made from bacterial spores - no stool involved. Bezlotoxumab, a monoclonal antibody given by IV, reduces recurrence by 10% when paired with antibiotics. These are becoming more common and may replace traditional FMT in the coming years.
Can you prevent C. diff with probiotics?
No. Major medical groups, including the Infectious Diseases Society of America, say there’s no strong evidence probiotics prevent C. diff. Some studies even suggest they might increase the risk of bloodstream infections in people with weakened immune systems. Don’t rely on yogurt, kefir, or supplements. The best prevention is smart antibiotic use.


12 Responses
Antibiotics are just profit machines for Big Pharma and hospitals don't care if you get C. diff as long as you come back for more treatment.
I had a bad case after a simple tooth extraction. Took me months to feel normal again. FMT was the only thing that helped. No joke.
This is so important 💪 I wish everyone knew how dangerous antibiotics can be. My mom went through 4 recurrences before FMT - now she’s back to hiking and gardening. Life-changing.
Anyone who still believes in fecal transplants hasn't read the peer-reviewed literature on microbial dysbiosis and the placebo effect in GI interventions. The 94% cure rate is cherry-picked from small cohorts with selection bias
As someone who’s worked in rural clinics across the Midwest, I’ve seen this firsthand. Patients don’t understand why they’re getting sick after antibiotics. We need better education - not just in hospitals but in pharmacies and GP offices too. FMT isn’t magic, it’s medicine.
And yes, clindamycin is still overprescribed for acne and sinus infections. It’s 2024. We should know better.
In Nigeria, we don’t have access to FMT or branded pills. We use local herbs and prayer. But I’ve seen people recover after stopping antibiotics early. Maybe the system is broken everywhere.
My sister had C. diff after a hip surgery. They gave her vancomycin for 10 days. She relapsed twice. Third time, they did FMT via capsule. She was back to work in a week. No more fear of bathrooms. This needs to be mainstream.
I’m just saying… what if the real problem is that doctors are too lazy to test for C. diff before prescribing? I got diagnosed after 3 weeks of diarrhea… and they still didn’t believe me until I begged. This system is broken.
They don’t test because it costs money and insurance won’t pay unless you’re in the hospital
Highly effective treatment. But access remains inequitable. In India, FMT is available only in top-tier hospitals. Most patients never hear of it. Awareness and affordability are critical.
Let’s be real: FMT is just a glorified poop enema. The FDA approved two products? That’s not science - that’s corporate lobbying. And don’t get me started on the lack of long-term data.
They’re selling you a miracle cure while the real solution - reducing unnecessary antibiotics - gets ignored. Same old story.