Blood Thinner & NSAID Risk Calculator
Calculate Your Risk
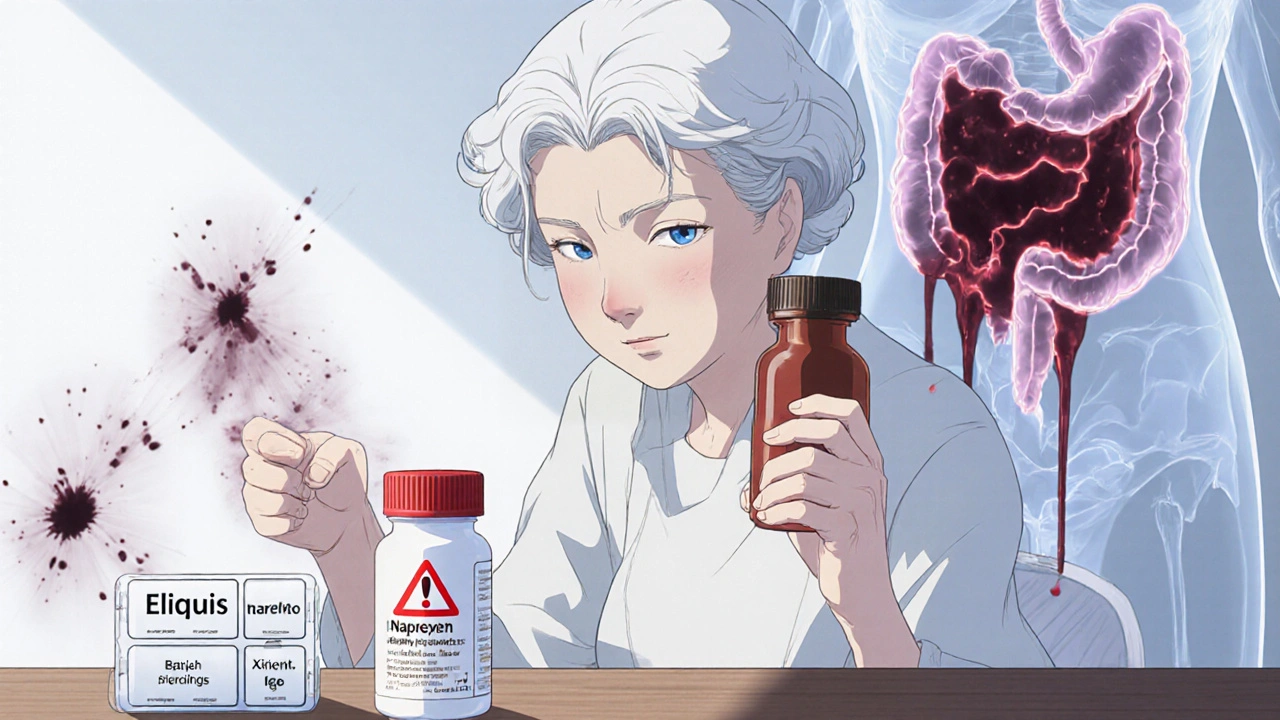
If you're taking a blood thinner like warfarin, Eliquis, or Xarelto, and you reach for ibuprofen or naproxen to ease a headache or sore knee, you're putting yourself at serious risk. This isn't a rare or theoretical concern-it’s a well-documented, life-threatening interaction that sends thousands to the emergency room every year. The truth is, blood thinners and NSAIDs don’t just mix poorly; they multiply danger in ways most people never expect.
How Blood Thinners and NSAIDs Work Together to Cause Bleeding
Blood thinners, or anticoagulants, don’t actually make your blood thinner. They slow down the clotting process so dangerous clots don’t form in your heart or legs. NSAIDs like ibuprofen, naproxen, and diclofenac work differently-they block enzymes that cause pain and inflammation, but they also stop platelets from sticking together. Platelets are the first responders when you cut yourself; without them, bleeding doesn’t stop easily. When you take both, you’re hitting your body’s clotting system from two sides. One drug delays the chemical cascade needed for clots to form. The other disables the cells that start the process. The result? A perfect storm for uncontrolled bleeding. This isn’t just about stomach bleeds. Studies show the risk extends to your brain, lungs, kidneys, and even your muscles. One major study tracking 200,000 patients found that combining NSAIDs with blood thinners made internal bleeding more than twice as likely. Naproxen? That raised the risk by over four times. Diclofenac? More than tripled it.Who’s Most at Risk-and Why It’s So Common
You might think this only affects older adults, but the truth is, it’s anyone on long-term anticoagulants. About 12 million Americans take blood thinners for conditions like atrial fibrillation, deep vein thrombosis, or after heart valve surgery. At the same time, over 17 million people use NSAIDs daily-many without a prescription. That’s a massive overlap. Older patients are especially vulnerable. Arthritis, back pain, and joint stiffness are common as we age. Many assume that because they’ve taken ibuprofen for years, it’s safe to keep using it-even with a blood thinner. But age brings thinner blood vessel walls, weaker stomach linings, and slower drug clearance. One study found that patients over 65 on warfarin who took NSAIDs had a 5.7 times higher risk of gastrointestinal bleeding than those who didn’t. Even worse, most people don’t know they’re at risk. A 2022 study showed only 43% of people on blood thinners were aware that NSAIDs could be dangerous. Nearly 7 out of 10 believed occasional use was fine. That’s a dangerous myth.Which NSAIDs Are the Worst?
Not all NSAIDs are created equal when it comes to bleeding risk. The data is clear:- Naproxen carries the highest risk-over four times higher bleeding rate compared to blood thinners alone.
- Diclofenac triples the risk and is particularly hard on the stomach lining.
- Ibuprofen is the most common OTC choice, but it still raises bleeding risk by nearly 80%.
- Aspirin, even in low doses, is an NSAID too. Many take it for heart protection, not realizing it adds to the danger when combined with other blood thinners.
What Happens When You Combine Them?
The consequences aren’t abstract. Real people end up in the ER with symptoms they didn’t see coming:- Dark, tarry stools or blood in vomit (signs of stomach bleeding)
- Unexplained bruising, especially large patches without injury
- Severe headaches, confusion, or vision changes (possible brain bleed)
- Unusual fatigue, dizziness, or rapid heartbeat (signs of anemia from internal blood loss)
What Should You Do Instead?
The safest pain reliever for people on blood thinners is acetaminophen (Tylenol). It doesn’t affect platelets or clotting. But even this has limits. Don’t exceed 3,000 mg per day-higher doses can harm your liver, especially if you drink alcohol or have existing liver issues. For chronic pain like arthritis, consider non-drug options:- Physical therapy and targeted exercises
- Heat or cold packs
- Topical creams with menthol or capsaicin
- Acupuncture or massage therapy
- Stopping the NSAID 2-3 days before any surgery or dental work
- Using the lowest effective dose for the shortest time possible
- Adding a stomach-protecting drug like omeprazole to reduce GI bleeding risk
- Checking your INR more frequently if you’re on warfarin
Why Doctors Still See This Mistake All the Time
You’d think this would be obvious by now. But here’s the problem: many patients don’t tell their doctors they’re taking over-the-counter meds. A patient might say, “I take my blood thinner,” but forget to mention the Advil they’ve been popping for back pain. Pharmacists don’t always catch it either-especially if the NSAID is bought without a prescription. Pharmacies don’t automatically flag interactions between warfarin and ibuprofen because the latter is sold over the counter. So the burden falls on you. And then there’s the frustration. One patient wrote on Harvard Health’s site: “It’s incredibly hard to manage arthritis pain when you can’t use the most effective meds.” That’s real. Chronic pain is exhausting. But the trade-off-internal bleeding, hospitalization, even death-isn’t worth it.
What You Need to Do Right Now
If you’re on a blood thinner:- Check every medication-even OTC pills, cold remedies, and supplements. Many contain NSAIDs under different names.
- Never start an NSAID without asking your doctor or pharmacist.
- Know the signs of bleeding-bruising, dark stools, dizziness, unexplained fatigue.
- Keep a list of all your medications and review it with your provider every 3-6 months.
- Ask about alternatives-acetaminophen, physical therapy, or topical treatments.
What’s Being Done to Fix This?
Health systems are starting to wake up. Some hospitals now include automated alerts in electronic records when a patient on a blood thinner tries to get an NSAID prescription. The FDA’s 2024 pain management initiative is pushing for safer alternatives tailored for this high-risk group. Researchers are exploring new drugs that reduce inflammation without affecting clotting-but those are still years away. For now, the solution is simple: avoid the combination. There’s no safe middle ground. If you’re on a blood thinner, NSAIDs are not a casual choice. They’re a medical decision-and one that should only be made with professional guidance.Can I take ibuprofen with warfarin if I only use it once in a while?
No. Even occasional use of ibuprofen while on warfarin increases your risk of bleeding. Studies show that just a few days of use can raise your INR and make your blood less able to clot. There’s no safe "occasional" dose when it comes to this combination.
Is aspirin safer than other NSAIDs when taking blood thinners?
No. Aspirin is an NSAID and interferes with platelet function just like ibuprofen or naproxen. In fact, many people take low-dose aspirin to prevent heart attacks, but combining it with another blood thinner significantly increases bleeding risk. Never take aspirin with a blood thinner unless your doctor specifically tells you to.
What about topical NSAIDs like gels or creams?
Topical NSAIDs (like diclofenac gel) are absorbed in much smaller amounts than pills, so they’re generally considered safer. But they’re not risk-free. If you have open wounds, large areas of skin, or kidney problems, even topical forms can enter your bloodstream enough to raise bleeding risk. Talk to your doctor before using them.
Can I take Tylenol (acetaminophen) with blood thinners?
Yes, acetaminophen is the safest over-the-counter pain reliever for people on blood thinners. But don’t exceed 3,000 mg per day. Higher doses can damage your liver, especially if you drink alcohol, have liver disease, or take other medications that affect liver function.
What should I do if I accidentally took ibuprofen while on a blood thinner?
Stop taking the NSAID immediately. Watch for signs of bleeding-unusual bruising, dark stools, dizziness, or fatigue. Call your doctor or go to urgent care if you notice any of these. You may need a blood test to check your INR or hemoglobin levels. Don’t wait for symptoms to get worse.
Are there any new pain medications for people on blood thinners?
There are no new drugs yet that are both effective for pain and completely safe with blood thinners. Researchers are working on them, but for now, acetaminophen and non-drug therapies remain the best options. Always check with your provider before trying anything new, even if it’s labeled "natural" or "herbal." Some supplements, like fish oil or garlic, also increase bleeding risk.

10 Responses
Bro, I took ibuprofen for my knee pain last week while on Eliquis… and now I’m here typing this with a bruise the size of a small pizza. 😅 Thanks for the wake-up call. Tylenol it is. 🙏
Honestly? This is why I stopped trusting OTC meds. I used to think ‘it’s just a pill’ - until my uncle ended up in the ER with a GI bleed after ‘just taking Advil for a few days.’ 🤦♀️ The system’s broken if we’re not getting better warnings. Even the bottle labels are vague. Someone needs to fix this.
Been on Xarelto for 4 years. Took naproxen once for a back flare-up. Didn’t feel anything… until I started passing black coffee-ground stuff. No pain, no warning. Just… blood. Ended up in the ER. Docs said I was 2 hours from needing a transfusion. I didn’t know. Nobody told me. Now I keep a list of everything I take. Even the ‘harmless’ stuff. 🤷♂️
USA is full of weak people who can’t handle pain without popping pills. In India, we’ve been using turmeric, ginger, and cold compresses for centuries. Why are you all so dependent on chemicals? 🤨 This isn’t medicine - it’s laziness. Your bodies are soft. Stop blaming the drugs. Fix your lifestyle.
THIS IS WHY AMERICA IS DYING. Big Pharma is killing us with silent killers. They don’t care if you bleed out - they make money off your ER visits. And the FDA? They’re asleep at the wheel. They knew this was coming. They let it happen. This isn’t an accident - it’s corporate negligence. 🚨
so i just found out my mom has been taking aleve with her warfarin for like 3 years… i think i might be in shock. she says she’s fine but i just checked her hemoglobin and it’s low. i’m gonna take her to the dr tomorrow. thank you for this post. i didn’t even know this was a thing 😅
You’re all missing the point. This isn’t about NSAIDs or blood thinners - it’s about your goddamn ignorance. You think you’re smart because you read a Reddit post? You don’t know what your INR is. You don’t track your meds. You don’t even know what ‘platelet aggregation’ means. You’re not patients - you’re walking time bombs with a pharmacy app on your phone. And now you’re all acting like victims? Get. A. Grip.
They’re hiding this on purpose. The CDC, the FDA, the pharma giants - they all know. That’s why they don’t put big red warnings on ibuprofen bottles. They want you to bleed quietly so they can sell you more blood tests, more hospital stays, more ‘safe’ alternatives that cost $120 a bottle. This is a money racket. I’ve seen the documents. They’re coming for your kidneys next.
It’s fascinating how we’ve outsourced our pain management to chemicals instead of listening to our bodies. We’ve forgotten that pain is information - not a problem to be erased. The real tragedy isn’t the bleeding - it’s that we’ve lost the patience to sit with discomfort, to move differently, to heal slowly. We want a pill for everything. And now we’re surprised when the system breaks? We built this. We’re not victims. We’re participants.
PERIOD. END. STATEMENT. NSAIDs + ANTICOAGULANTS = MULTIPLE-ORGAN FAILURE RISK PROFILE: EXTREME. DO NOT COMBINE. DO NOT IGNORE. DO NOT ASSUME ‘OCCASIONAL’ IS SAFE. THE DATA IS NON-NEGOTIABLE. THE EVIDENCE IS OVERWHELMING. THE CONSEQUENCES ARE IRREVERSIBLE. YOU ARE NOT A STATISTIC - YOU ARE A LIABILITY TO YOURSELF AND YOUR HEALTHCARE SYSTEM. CONSULT YOUR PHARMACIST. NOW. BEFORE IT’S TOO LATE.