Why do so many patients stick with expensive, brand-name drugs when a cheaper, equally effective generic is right there? It’s not about ignorance. It’s not about laziness. It’s about something deeper - something baked into how our brains work. Behavioral economics explains why people don’t act like rational robots when it comes to their health, especially when choosing medications.
It’s Not About Cost - It’s About Fear
Most people assume that if a drug costs less, patients will switch. But data says otherwise. In one study, 68% of patients kept taking their current medication even when a better-priced alternative was available and proven to work just as well. Why? Fear. Not fear of the disease - fear of change. The brain treats uncertainty like a threat. Switching drugs feels risky, even if the science says it’s safe. This is called risk aversion. Your brain weighs the pain of a potential bad outcome (side effects, failure) much more heavily than the gain of saving money. Add to that loss aversion: people hate losing something they already have. Even if the current drug has side effects or high copays, patients feel like they’re losing control or safety if they switch. One study found that patients were more motivated to avoid losing a $50 rebate than they were to gain a $50 discount. That’s why rebate programs tied to adherence work better than simple discounts.The Power of Defaults
Imagine you’re a doctor. You open your electronic health record to prescribe a medication. The top three options are listed in a specific order. The first one? A brand-name drug. The second? A generic. The third? Another brand-name drug. Chances are, you’ll pick the first one. Not because it’s best. Because it’s first. This is the default effect. Humans are lazy decision-makers. We take the path of least resistance. In a 2012 study, when hospitals changed their default prescriptions in EHR systems to favor lower-cost alternatives during drug shortages, appropriate substitutions jumped by 37.8%. No lectures. No training. Just a simple reordering of options. Pharmaceutical companies know this. That’s why they pay to be listed first in formularies. Payers and hospitals are starting to fight back - by setting defaults that nudge toward cost-effective, evidence-based choices. But it’s still rare. Most systems still prioritize what’s easiest for the pharmacy, not what’s best for the patient.Framing Matters More Than Facts
How you say something changes how people feel about it. A vaccine that’s “95% effective” feels safer than one that’s “5% ineffective.” The numbers are identical. But the brain responds to the frame. In a 2021 trial, framing flu shot messages as “95% of people avoid hospitalization” led to an 18.4 percentage point increase in uptake compared to messages about risk. The same trick works with prescriptions. Saying “This medication reduces your chance of a heart attack by 30%” lands differently than “There’s still a 70% chance you’ll have a heart attack.” Doctors and pharmacies often miss this. They give patients lists of side effects, risks, and stats - overwhelming them with information. But behavioral economics shows that clarity and positive framing win every time. A simple message like “Taking this daily keeps you out of the hospital” works better than a 10-point bullet list.Why Patients Forget - And How to Help
You know how you forget to take your vitamins? Now imagine you’re on five medications. You have diabetes, high blood pressure, cholesterol, arthritis, and depression. Each has its own schedule. Some need to be taken with food. Others on an empty stomach. Some once a day. Others twice. One at night. One in the morning. This is polypharmacy. And it’s a nightmare for adherence. Research shows each extra pill cuts adherence by 8.3%. For someone on six meds? That’s nearly half the chance they’ll take everything correctly. The solution isn’t more reminders. It’s smarter ones. A 2021 study tested two types of SMS texts:- “Don’t forget to take your pill.”
- “Don’t lose your streak!”
Social Pressure Works - Even in Health
We care what others think. Even when we say we don’t. In an HIV treatment program, clinics put up posters showing monthly adherence rates. Not names. Just numbers: “This month, 89% of our patients took their meds as prescribed.” Adherence jumped by 22.3%. Why? Because people didn’t want to be the outlier. They didn’t want to be the one who fell behind. This is social norms in action. We follow the crowd. Even in something as personal as taking pills. That’s why peer support groups, community health champions, and even family reminders can be more effective than clinical advice alone. Pharmaceutical companies are starting to use this in patient support programs. Instead of just sending emails, they’re building communities where patients share wins. “I took all my meds this week!” becomes a badge. A small thing. But powerful.Why Education Alone Fails
For decades, the go-to solution for poor adherence was education. Brochures. Videos. One-on-one counseling. But here’s the truth: after 44 studies reviewed in 2022, traditional education improved adherence by only 5-8%. That’s barely better than doing nothing. Behavioral interventions? They improved prescribing and adherence in 92% of studies. The best? Defaults. Then social norms. Then framing. Education? Last. Why? Because knowing something isn’t the same as doing it. You know smoking is bad. You still might smoke. You know exercise helps. You still might skip it. Health decisions aren’t made in a classroom. They’re made in the chaos of daily life - when you’re tired, stressed, confused, or overwhelmed. Behavioral economics doesn’t try to fix knowledge. It fixes the environment. It makes the right choice the easiest choice.Barriers No One Talks About
Not all patients are the same. Some barriers are invisible. - Asymptomatic conditions: If you don’t feel sick, why take a pill? Blood pressure meds? Cholesterol pills? 32.7% lower adherence than for drugs that relieve pain or symptoms. - Negative beliefs: “Medications are poison.” “Doctors just want to make money.” These beliefs explain 41.2% of why people stop taking their meds. - Mental health: Depression cuts adherence by 28.4%. Anxiety by 22%. If you’re struggling to get out of bed, remembering to take five pills feels impossible. One-size-fits-all programs fail here. You can’t nudge someone with severe depression the same way you nudge someone with mild anxiety. Tailoring matters. A patient who believes meds are harmful needs trust-building, not reminders. Someone with depression needs simplified routines, not complex apps.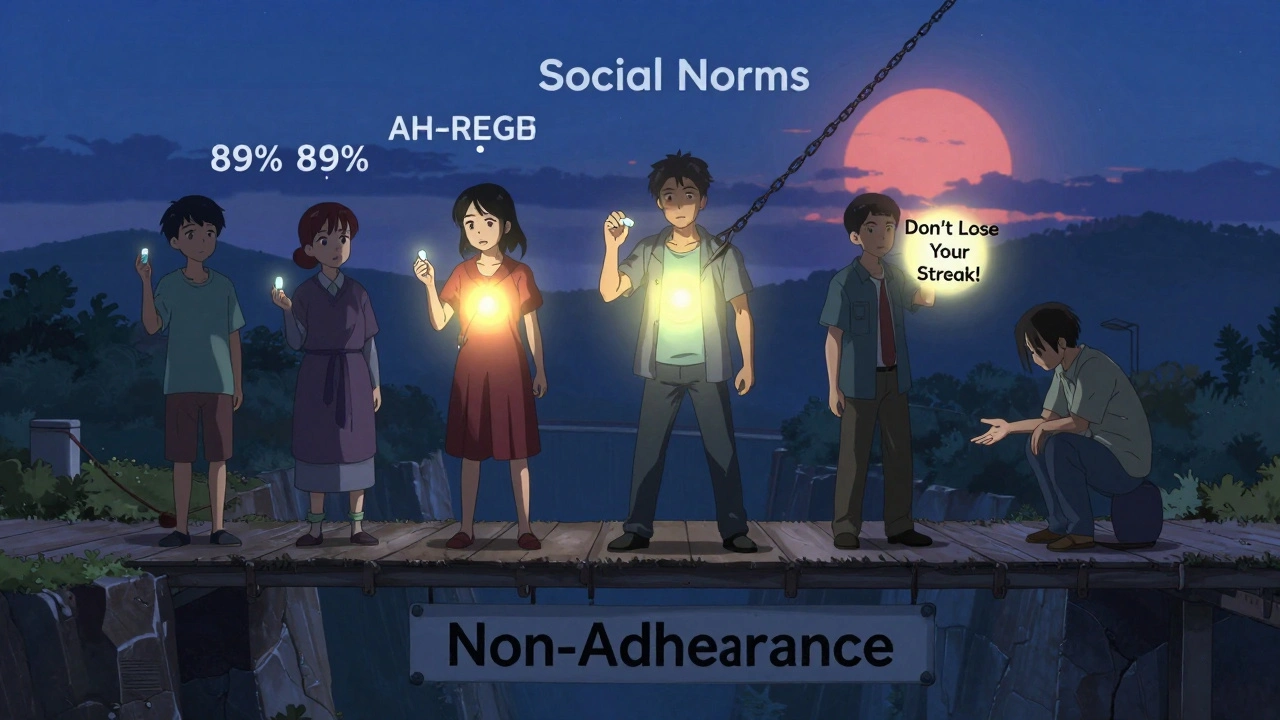


9 Responses
People stick with brand names because they trust the logo not the science
Simple as that
This whole post is woke nonsense. Americans don't need behavioral nudges. We need less regulation and more competition. If generics were truly equal, they'd dominate without all this psychobabble.
I've been thinking about this a lot since my mom got switched to a generic blood pressure med last year. She was terrified it wouldn't work even though the doctor explained it was identical. She kept checking her BP every morning like it was a ritual. After two weeks she started feeling better but still insisted it was because she 'got lucky' with the new pill. It's not just fear of side effects-it's identity. The brand name became part of her sense of control. When the pharmacist changed the label, she felt like her routine was being stolen. The default effect in EHRs is real, but so is the emotional attachment people build to their meds. We treat pills like talismans. And honestly? Maybe we should. If believing in the blue pill with the big logo helps someone take it daily, who are we to take that away? The real problem isn't the patient-it's the system that makes them feel like they need a lucky charm to stay alive.
You think this is unique to America? In Nigeria, people pay triple for imported drugs because they believe 'foreign medicine' works better. Even when local generics are FDA-approved. The fear isn't just psychological-it's colonial. We were taught for generations that Western drugs are sacred. Now we're stuck with this mental inheritance. And yes, the default effect? It's everywhere. Pharmacies here put the most expensive brand first. No one questions it. Because why would you? The doctor didn't say anything. The pharmacist didn't say anything. So we assume the top one is the best. This isn't behavioral economics. This is cultural trauma dressed up as choice.
I work in a community clinic and I see this every day. One woman came in crying because she stopped her cholesterol med after her husband died. She said, 'I don't need it anymore. I'm not taking care of myself now.' It wasn't about cost or fear-it was grief. She didn't have the energy to fight the system anymore. We started sending her a simple text every morning: 'You got this. One pill today.' No science. No stats. Just that. She started taking it again in two weeks. The real nudge wasn't the text-it was the fact that someone remembered she was still here. Sometimes the most powerful behavioral tool isn't a default or a rebate. It's someone saying, 'I see you.'
This is why India is better than US. We dont need fancy psychology. We just take what doctor says. No whining about brand names. No rebates. No texts. Just take the pill. If you cant handle it then dont complain when you get sick. Americans think everything needs a nudge. We just do it. No drama
I appreciate how this breaks down the psychology behind adherence. I think the most overlooked point is the mental health connection. Depression doesn't just make you forget pills-it makes you feel like you don't deserve to be healthy. That's not a nudge problem. That's a systemic failure. We're treating symptoms with behavioral hacks while ignoring the root causes of despair. Maybe the real nudge should be: 'Your life matters enough to be supported.' Not just 'Don't lose your streak.'
Everyone here is missing the real issue. People don't take meds because they're lazy or scared. They take them because they're forced to. The real problem is the medical industrial complex. Pharma companies control everything. They pay doctors. They control formularies. They make sure generics are hard to access. This whole post is just a distraction. Stop blaming patients. Start blaming the corporations that profit from confusion and fear. And yes, I've seen it firsthand. My cousin got switched to a generic and the pharmacy refused to fill it because the insurer didn't approve it. No one told her why. She just stopped taking it. It wasn't her fault. It was the system.
This is manipulation not medicine