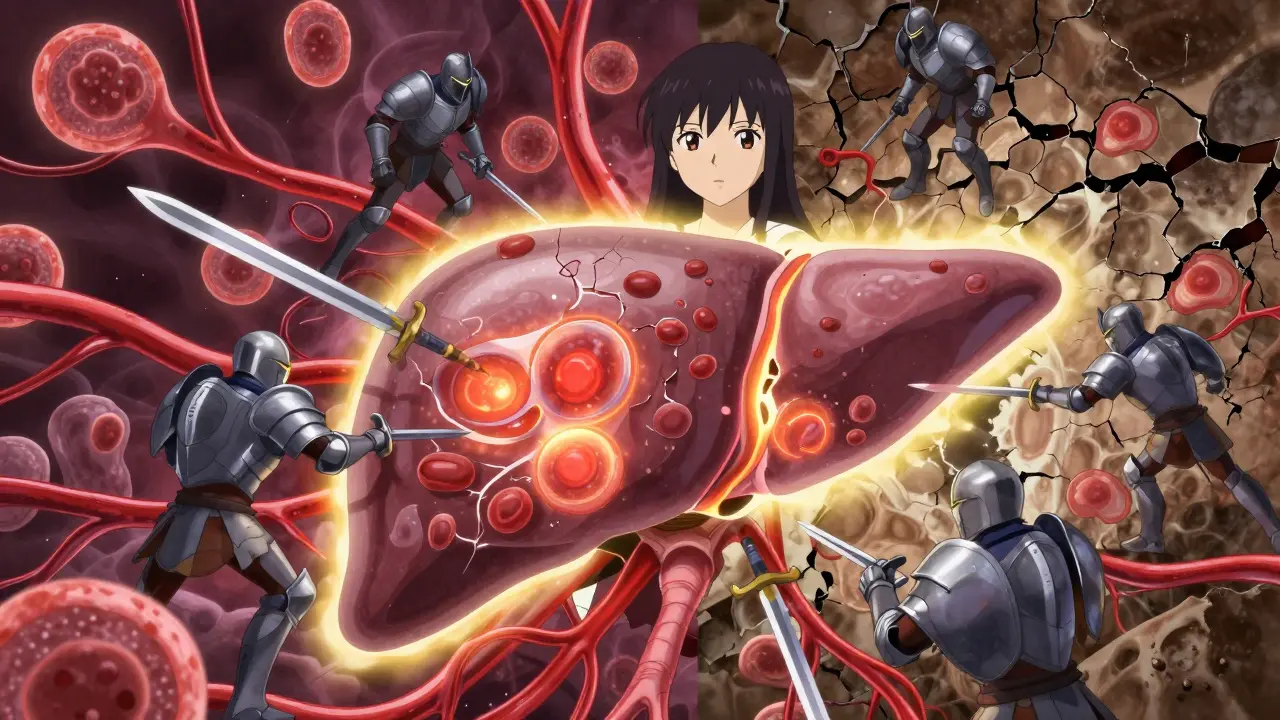
Autoimmune hepatitis is not just another liver problem. It’s when your own immune system turns on your liver, attacking healthy cells like they’re invaders. This isn’t caused by alcohol, viruses, or fatty foods. It’s an internal betrayal - and it can quietly destroy your liver over years if left unchecked.
What Happens When Your Immune System Attacks Your Liver
In autoimmune hepatitis, immune cells mistake liver cells for foreign threats. They swarm in, release inflammatory chemicals, and start breaking down tissue. This leads to inflammation - and over time, scarring. The process is called interface hepatitis, where immune cells chew through the border between liver tissue and blood vessels. Left alone, this turns into fibrosis, then cirrhosis, and eventually liver failure.
Unlike hepatitis B or C, which come from viruses, autoimmune hepatitis has no external trigger. It’s not contagious. It’s not caused by drinking. It’s an autoimmune disorder - similar to rheumatoid arthritis or lupus - but focused on the liver. And unlike other liver diseases that target bile ducts (like PBC or PSC), autoimmune hepatitis goes straight for the hepatocytes, the main working cells of the liver.
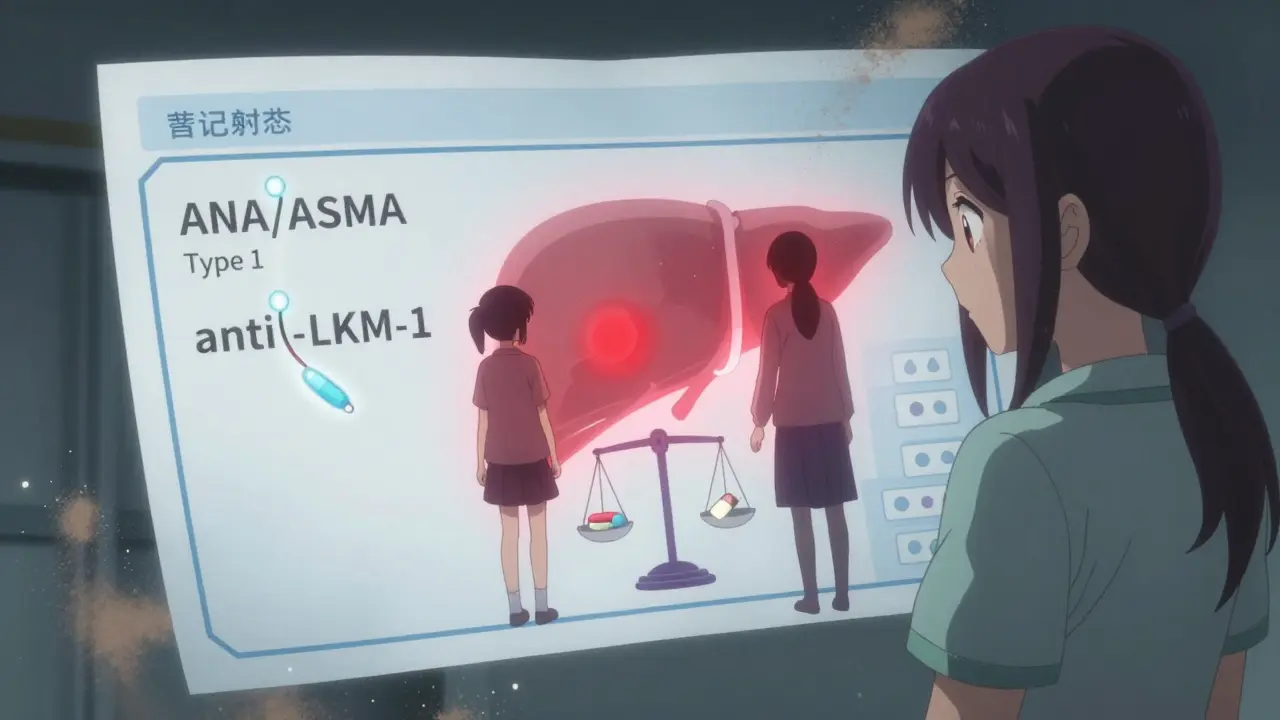
Two Main Types - And Who Gets Them
There are two main types of autoimmune hepatitis, and they affect different people in different ways.
- Type 1 is the most common - making up 80-90% of cases in North America and Europe. It usually shows up in teens and young adults, and women are far more likely to get it than men - about 3.6 times more often.
- Type 2 is rarer and mostly seen in children between ages 2 and 14. It’s even more skewed toward girls, with a female-to-male ratio of 8:1.
The difference isn’t just age or gender. Each type has its own antibody signature. Type 1 often shows antinuclear antibodies (ANA) or anti-smooth muscle antibodies (ASMA). Type 2 is marked by anti-LKM-1 or anti-LC-1 antibodies. These aren’t just labels - they help doctors confirm the diagnosis and rule out other conditions.
How It Shows Up - Symptoms You Can’t Ignore
Some people feel fine until a routine blood test reveals liver damage. Others crash into symptoms hard. There’s no single pattern.
- 25-35% of patients come in with sudden, flu-like symptoms - fatigue, nausea, jaundice - mimicking viral hepatitis.
- 40-50% have a slow, creeping illness: tired all the time, achy joints, unexplained weight loss.
- 15-20% show no symptoms at all. Their liver enzymes are just off during a checkup.
Lab tests usually show the same red flags:
- ALT and AST levels 5-10 times higher than normal
- IgG levels over 1.5 times the upper limit
- Elevated bilirubin in advanced cases
And yes - fatigue is the worst part for most. A 2022 survey of over 1,000 patients found that 78% ranked constant exhaustion as their most disabling symptom. Joint pain, mood swings, and insomnia aren’t side effects - they’re part of the disease.
Diagnosis: Ruling Out the Rest
There’s no single test for autoimmune hepatitis. Diagnosis is a puzzle. Doctors look for:
- Blood tests showing elevated liver enzymes and IgG
- Specific antibodies (ANA, ASMA, LKM-1, etc.)
- Exclusion of viral hepatitis, alcohol use, and drug-induced injury
- A liver biopsy showing lymphoplasmacytic infiltration and interface hepatitis
The Revised International AIH Group Scoring System, updated in 2022, is the gold standard. It uses a point system to weigh lab results, antibodies, and biopsy findings. When used by experienced hepatologists, it’s 97% specific - meaning it rarely mistakes something else for AIH.
But here’s the catch: 15-20% of cases are misdiagnosed as drug-induced liver injury. That’s because some medications - like statins, antibiotics, or even herbal supplements - can cause similar liver damage. If you’ve started a new drug before symptoms appeared, your doctor will need to rule that out carefully.
Standard Treatment: Suppressing the Attack
The goal isn’t to cure - it’s to stop the immune system from destroying your liver. And the treatment is powerful: immunosuppressants.
The first-line therapy is a combo of prednisone (a corticosteroid) and azathioprine. Prednisone shuts down inflammation fast. Azathioprine keeps the immune system quiet long-term.
Typical starting dose: 0.5-1 mg/kg of prednisone daily (up to 60 mg), plus 50 mg of azathioprine. Within 3-6 months, most patients see their liver enzymes drop. Full remission - meaning normal enzyme and IgG levels - takes 18-24 months for 60-65% of people.
But there’s a cost. Prednisone isn’t gentle. Side effects include:
- Weight gain (reported by 82% of users)
- Insomnia (67%)
- Mood swings and anxiety (58%)
- Bone thinning - osteoporosis risk doubles
That’s why doctors try to taper prednisone down as soon as possible. Azathioprine becomes the mainstay. Some patients need to stay on low-dose azathioprine for life.
What If Treatment Doesn’t Work?
About 10% of patients don’t respond to standard therapy. These are called treatment-refractory cases. Their liver enzymes stay high, inflammation continues, and fibrosis creeps forward.
For them, second-line drugs are used:
- Mycophenolate mofetil - effective in 70-80% of azathioprine-intolerant patients
- Rituximab - a biologic that targets B-cells, now in phase 3 trials
- Vedolizumab - being tested for gut-liver immune connection
And for those who progress to end-stage liver disease? Liver transplant. Autoimmune hepatitis is the fourth leading reason for adult liver transplants in the U.S., accounting for 6.2% of all transplants in 2022. The good news? Transplant success rates are high - over 90% survive five years post-transplant.
Living With It: Daily Realities
Managing autoimmune hepatitis isn’t just about pills. It’s a lifestyle shift.
- You need blood tests every 2-4 weeks during the first few months of treatment.
- Take azathioprine at the same time every day - missing doses increases relapse risk.
- Calcium and vitamin D supplements are non-negotiable to protect bone density.
- Get flu shots and pneumonia vaccines - your immune system is suppressed.
- Avoid alcohol completely - even small amounts speed up liver damage.
And mentally? It’s heavy. A 2022 survey found 71% of patients live with constant anxiety about disease progression. Many report job loss or reduced hours because fatigue and brain fog make work impossible.
But there are success stories. One patient, Sarah K., shared: “My ALT dropped from 480 to 32 in six weeks. I went from barely able to walk to hiking again. It wasn’t easy - but it was worth it.”
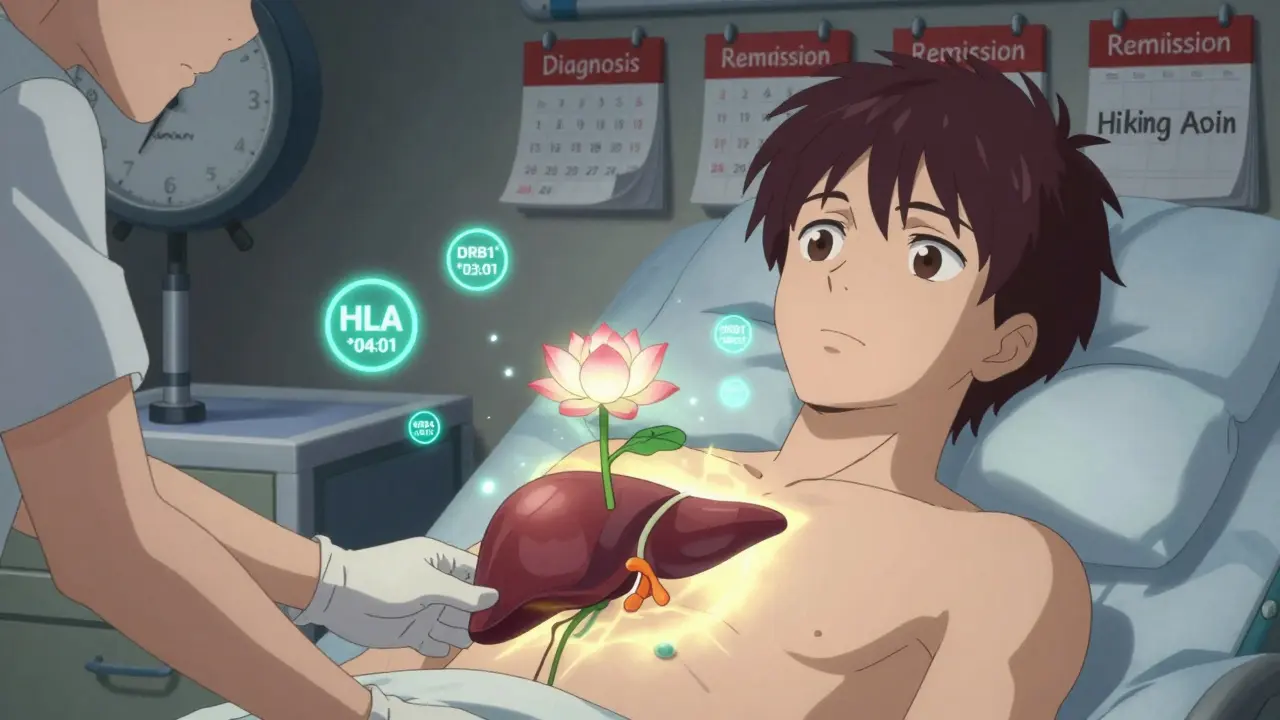
The Future: Precision Medicine on the Horizon
Research is moving fast. In 2023, the International Autoimmune Hepatitis Group added a new antibody - anti-SLA/LP - to diagnostic criteria. It boosts accuracy to 99%.
And the biggest shift? Genetic profiling. Scientists now know that certain HLA gene variants - especially HLA-DRB1*03:01 and *04:01 - strongly predict who gets AIH and how they respond to treatment. In the next 5-7 years, doctors may use genetic tests to pick the right drug for the right person. Imagine: no trial-and-error. No 6 months of side effects. Just the right dose, from day one.
Obeticholic acid, a drug originally for PBC, got orphan drug status in Europe in 2022 after showing 45% remission rates in early trials. It’s not approved yet - but it’s coming.
Why Early Diagnosis Is Everything
Untreated autoimmune hepatitis is deadly. Without treatment, only 10% of patients survive 10 years. With treatment? Survival jumps to 94%.
That’s not a statistic. That’s a life. A career. A future. A parent who gets to see their child graduate. A person who can walk without exhaustion.
If you’ve been told your liver enzymes are high and no virus was found - don’t dismiss it. Ask for antibody testing. Ask for a biopsy. Push for answers. This disease doesn’t announce itself. It creeps. But it can be stopped - if caught in time.
Is autoimmune hepatitis the same as viral hepatitis?
No. Viral hepatitis is caused by infections - like hepatitis B or C - and is treated with antivirals. Autoimmune hepatitis is caused by your immune system attacking your liver. It requires immunosuppressants, not antivirals. The symptoms can look similar, but the treatments are completely different.
Can autoimmune hepatitis be cured?
There’s no cure yet. But with proper treatment, most people achieve remission - meaning the immune system stops attacking the liver. Many can live normal lifespans with low-dose medication. Some may eventually stop treatment, but most need lifelong monitoring.
Why do I need a liver biopsy if my blood tests are clear?
Blood tests show liver stress, but not the cause. A biopsy looks at actual liver tissue. It can confirm inflammation patterns unique to autoimmune hepatitis, rule out other diseases like fatty liver or cancer, and show how much scarring has already happened. It’s the only way to get a definitive diagnosis.
Are there new drugs coming for autoimmune hepatitis?
Yes. While prednisone and azathioprine have been the standard for decades, new drugs are in trials. Rituximab, vedolizumab, and obeticholic acid are showing promise. Obeticholic acid, in particular, achieved 45% remission in early trials - nearly double the placebo rate. These aren’t approved yet, but they’re close.
Can I drink alcohol if I have autoimmune hepatitis?
No. Alcohol adds direct toxicity to an already damaged liver. Even small amounts can accelerate scarring and increase your risk of cirrhosis. Complete abstinence is required for all patients with autoimmune hepatitis, regardless of disease stage.
What’s the risk of liver cancer with autoimmune hepatitis?
The risk is low if you’re in remission. But if the disease progresses to cirrhosis, your risk of hepatocellular carcinoma (liver cancer) increases significantly. That’s why regular monitoring - including ultrasound every 6 months - is critical once fibrosis develops.

2 Responses
Let me just say this outright: if you're not getting tested for ANA and ASMA after unexplained liver enzyme spikes, you're being negligent. I've seen too many people in India dismissed as 'just stressed' or 'fatigue from work'-until their ALT hits 1000 and they're on a transplant list. This isn't a suggestion. It's a medical emergency disguised as a slow burn. No, you don't need to be drunk or eat junk to destroy your liver. Your own immune system will do it for free, no subscription required. And yes, women are disproportionately affected-not because they're 'weaker' but because their immune systems are more reactive. Stop normalizing fatigue. Stop brushing off joint pain. This isn't normal aging. It's an internal war, and if you're not fighting it with steroids and azathioprine, you're surrendering.
And for the love of God, stop drinking. Even one beer. Ever. I don't care if you're 'only having it socially.' Your liver doesn't care about your social calendar. It's already under siege. You don't get to choose when you die. But you do get to choose whether you give it a fighting chance.
Okay but like... have you even read the 2022 revised scoring system? Like, the whole thing is built on this 97% specificity metric-which is wild because most autoimmune stuff is diagnosed by process of elimination. I mean, come on. The fact that we're now using anti-SLA/LP as a diagnostic marker? That's like, next-gen stuff. And don't even get me started on HLA-DRB1*03:01. Like, if you have that variant and elevated IgG? You're basically genetically predestined for AIH. It's not even a guess anymore. It's a prediction. And obeticholic acid? 45% remission? That's not a drug. That's a miracle. The fact that we're still using prednisone as first-line in 2024 is kinda embarrassing honestly. Like, we have precision medicine tools and we're still throwing steroids at people like it's 1987.